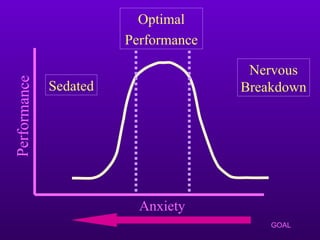
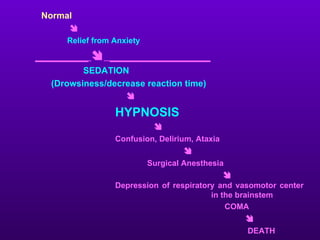
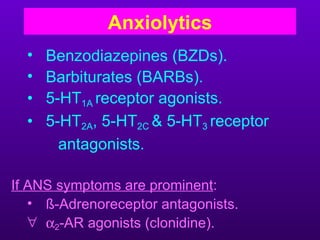
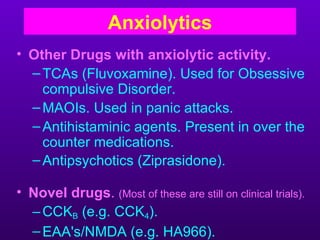
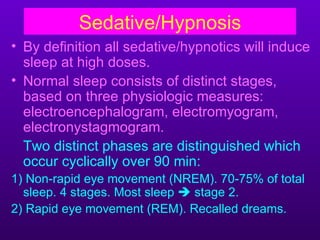
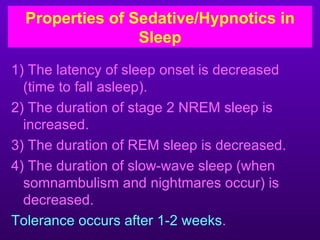
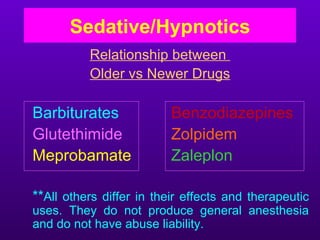
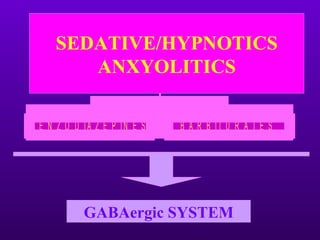
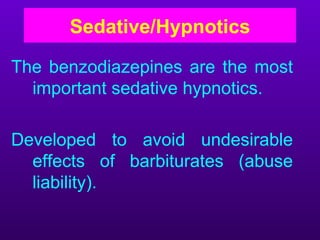
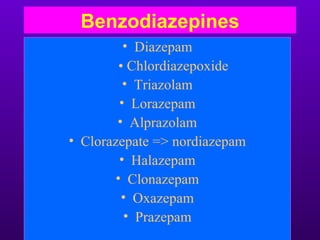
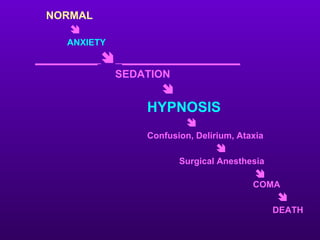
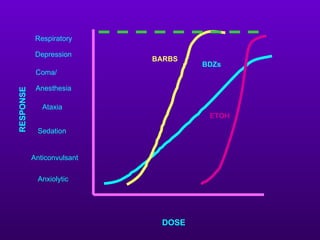
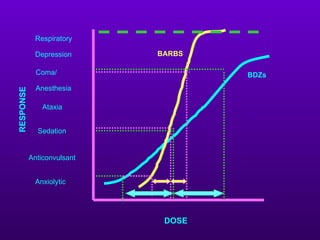
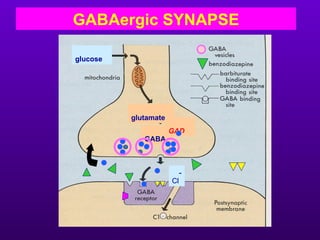
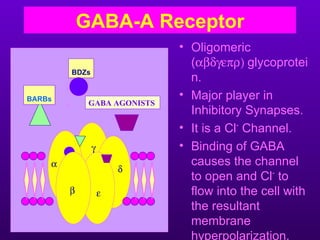
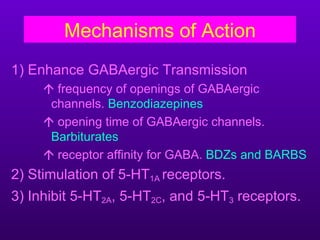
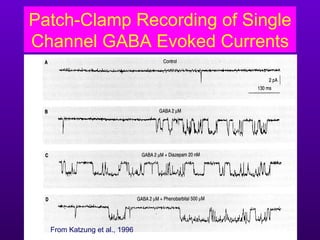
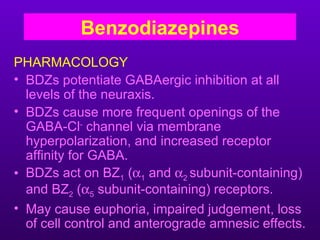
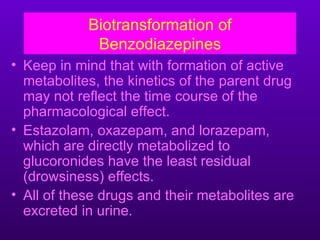
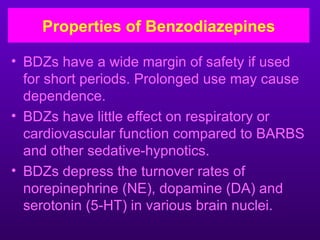
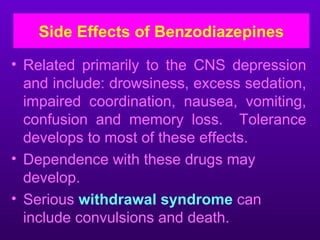
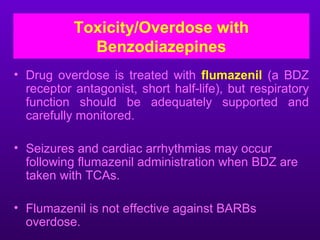
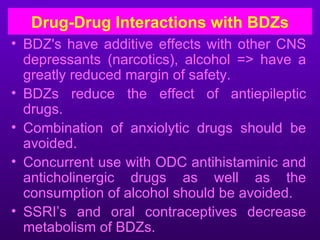
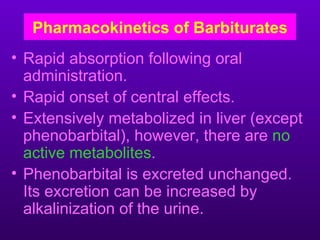
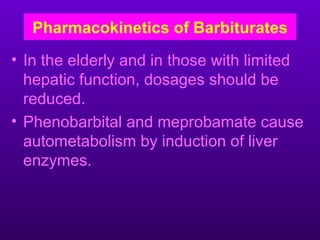
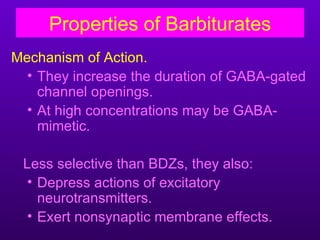
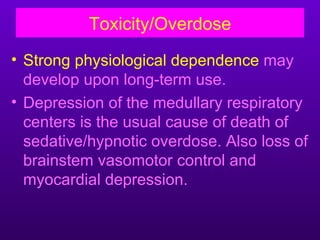
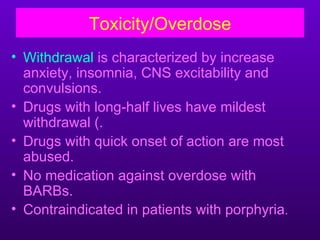
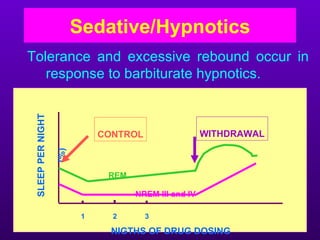
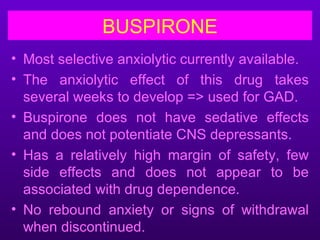
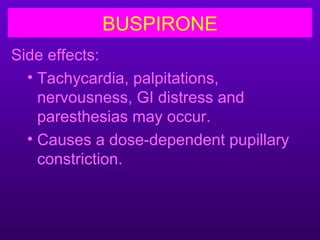
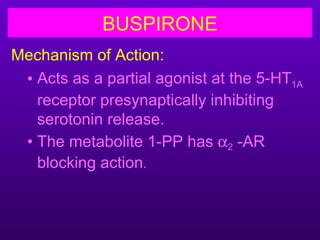
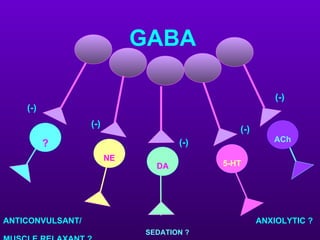
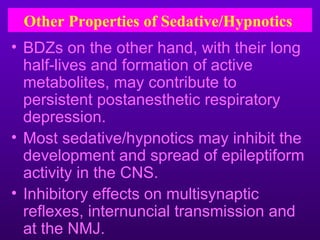
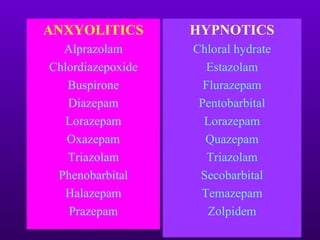
This document discusses sedative/hypnotics and anxiolytics. It begins by explaining how these drugs work in the nervous system, producing sedation, hypnosis, and effects ranging from confusion to coma and death depending on dose. It then focuses on benzodiazepines and barbiturates, the two major classes of these drugs. Both act by enhancing GABAergic transmission but differ in their mechanisms and properties. Benzodiazepines are generally safer with less respiratory depression but can cause dependence, while barbiturates have greater toxicity and abuse potential. The document emphasizes using these drugs only short-term to avoid adverse effects.