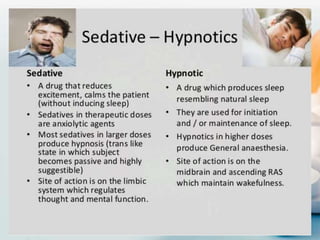
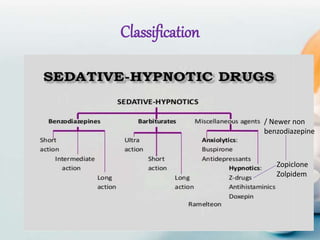
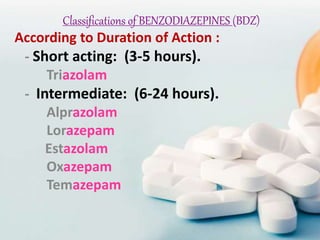
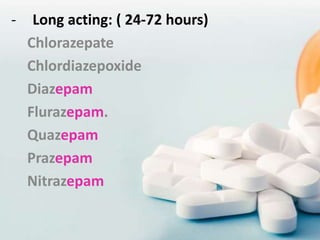
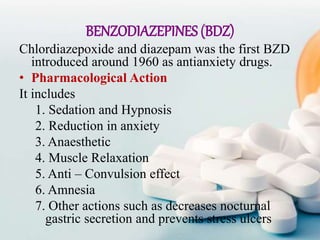
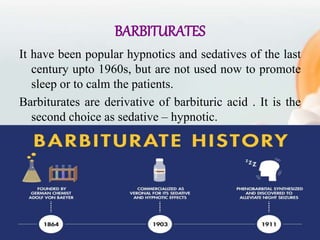
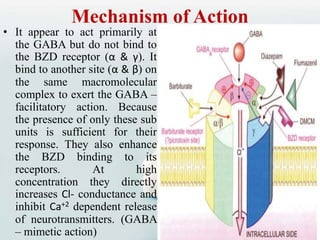
The document provides an overview of sedatives and hypnotics, distinguishing between sedatives that calm without inducing sleep and hypnotics that induce sleep. It details various drug classifications, pharmacological actions, mechanisms of action, pharmacokinetics, adverse effects, and nursing responsibilities related to benzodiazepines and barbiturates. Additionally, it discusses non-benzodiazepine hypnotics, including their uses, efficacy, and potential side effects.