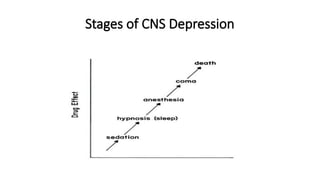
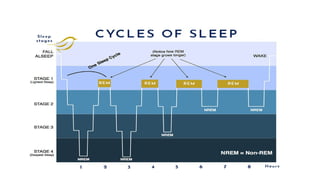
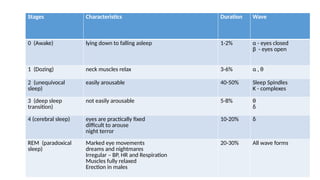
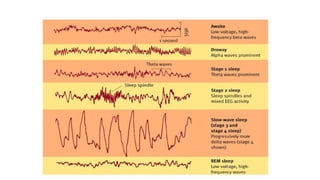
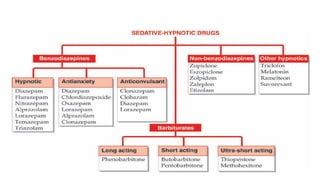
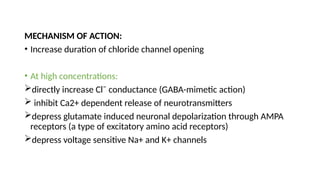
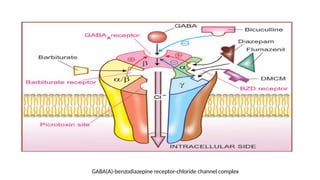
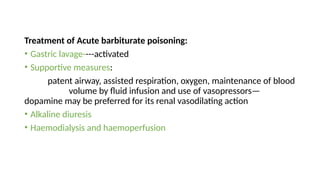
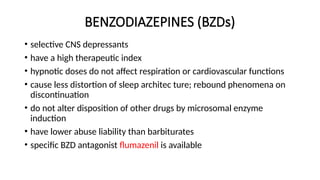
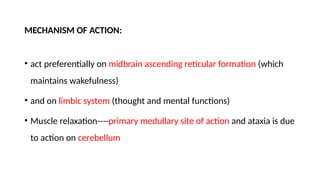
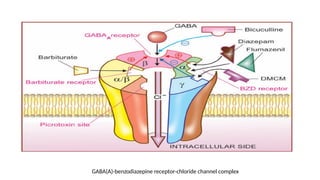
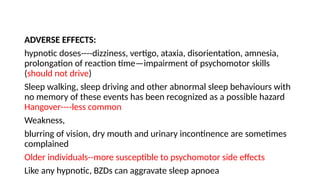
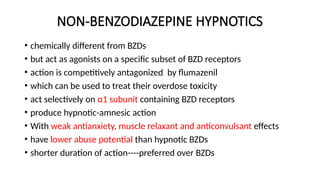
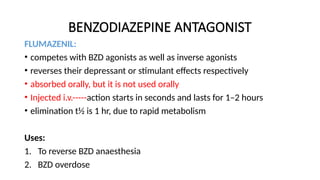
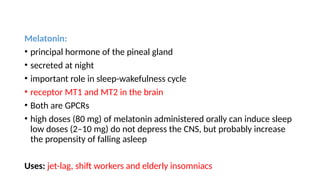
The document provides an overview of sedative-hypnotics, including their definitions, types, mechanisms, and pharmacological effects, with a focus on barbiturates and benzodiazepines. It discusses the various stages of CNS depression, side effects, uses, and treatment of barbiturate poisoning, along with alternative hypnotics like non-benzodiazepine agents and melatonin. Additionally, it covers newer medications such as ramelteon and suvorexant, highlighting their roles in sleep regulation.