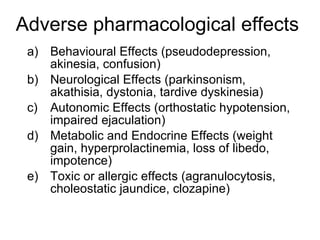
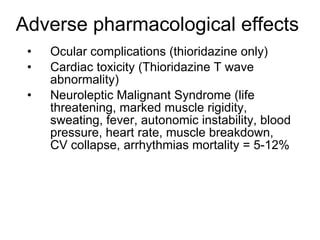
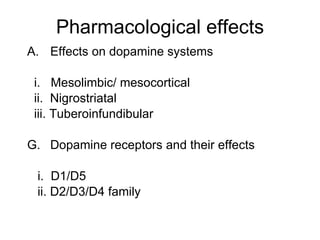
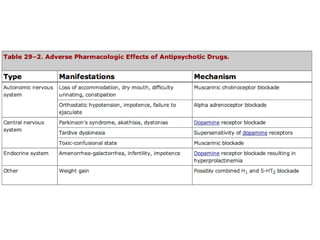
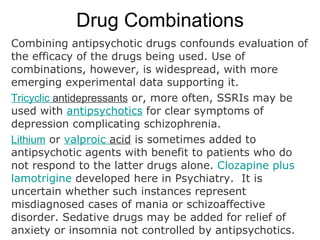
This document discusses antipsychotic drugs and their mechanisms and uses. It covers the dopamine hypothesis of schizophrenia and how antipsychotics work by blocking dopamine receptors. It describes the differences between typical and atypical antipsychotics, with atypicals having less motor side effects and effects on negative symptoms. The document outlines adverse effects of antipsychotics and provides clozapine as an example of an atypical drug, noting its superior efficacy but risks of side effects requiring blood monitoring.
![CLOZAPINE: AN EXAMPLE OF AN ATYPICAL NEUROLEPTIC
•Clozapine (sold as Clozaril, Leponex, Fazaclo; Gen-Clozapine in Canada) was the
first of the atypical antipsychotics to be developed. It was approved by the United
States Food and Drug Administration (FDA) in 1989 and is the only FDA-approved
medication indicated for treatment-resistant schizophrenia and for reducing the risk
of suicidal behaviour in patients with schizophrenia. [dubious – discuss]
•Clozapine has been shown to be superior in efficacy in treating schizophrenia.
Were it not for its side effects it would be first line treatment; however the rare but
potentially lethal side effects of agranulocytosis and myocarditis relegate it to third-
line use. Furthermore it may rarely lower seizure threshold, cause hepatic
dysfunction, weight gain and be associated with type II diabetes. More common side
effects are predominantly anticholinergic in nature, with dry mouth, sedation and
constipation. It is also a strong antagonist at different subtypes of adrenergic,
cholinergic, histaminergic and serotonergic receptors.
•Safer use of clozapine requires weekly blood monitoring for around five months
followed by four weekly testing thereafter. Echocardiograms are recommended
every 6 months to exclude cardiac damage.](https://image.slidesharecdn.com/antipsychotics07web-090716160745-phpapp01/85/Antipsychotics-07web-10-320.jpg)
![Charlton BG. If 'atypical' neuroleptics did not
exist, it wouldn't be necessary to invent them:
perverse incentives in drug development,
research, marketing and clinical practice.
Medical Hypotheses. 2005; 6: 1005-9.
There is now ample evidence to suggest that neuroleptics (aka. anti-psychotics and major
tranquillizers) are dangerous drugs, and patients’ exposure to them should be minimized
wherever possible. This clinical imperative applies whether neuroleptics are of the traditional
type or atypical variety, albeit for different reasons since the traditional agents are neurotoxic
while atypicals are mainly metabolic poisons. Usage of traditional neuroleptics seems indeed
to be declining progressively, but the opposite seems to be happening for ‘atypicals’, and new
indications for these drugs are being promoted. Yet the atypical neuroleptics are a category of
pharmaceuticals which are close to being un-necessary since there are safer, cheaper and
pleasanter substitutes such as benzodiazepines and the sedative antihistamines (eg.
promethazine).
“In terms of therapeutic value, it therefore seems likely that 'atypicals' are merely an unusually dangerous
way of sedating patients. In therapeutic terms these drugs therefore represent a significant backward step.
Rationally, the atypicals should now be dropped and replaced with safer sedatives. Potential neuroleptic-
substitutes which already exist would include benzodiazepines and sedative antihistamines such as
promethazine [4,8].”](https://image.slidesharecdn.com/antipsychotics07web-090716160745-phpapp01/85/Antipsychotics-07web-11-320.jpg)