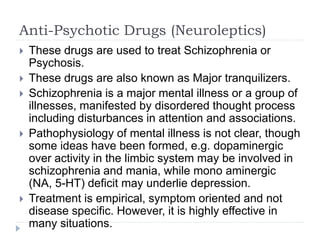
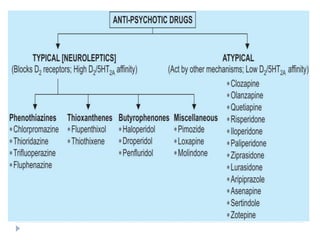
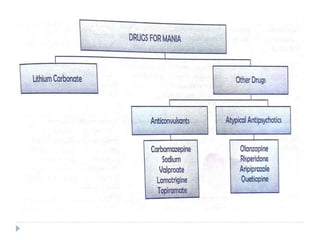
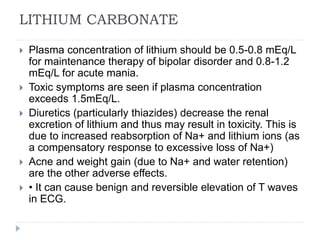
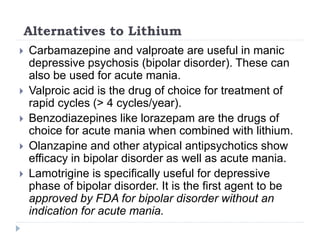
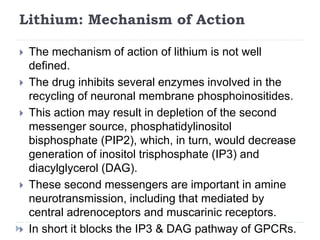
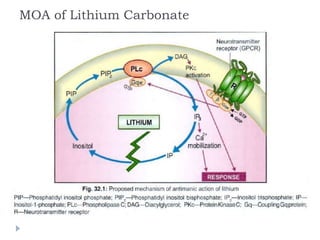
This document summarizes various psychopharmacological agents. It discusses anti-anxiety drugs like benzodiazepines which act by increasing GABA activity. Anti-psychotic drugs for treating schizophrenia are also covered, noting they work by blocking dopamine D2 receptors. Lithium is described as the standard treatment for bipolar disorder, stabilizing mood by inhibiting inositol monophosphate. Adverse effects of these classes of drugs are also briefly outlined.