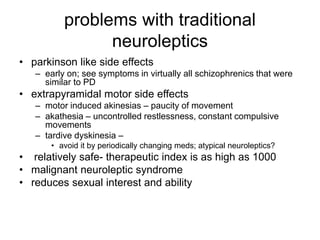
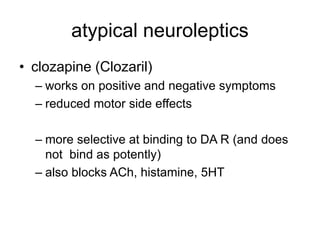
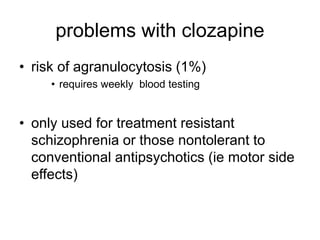
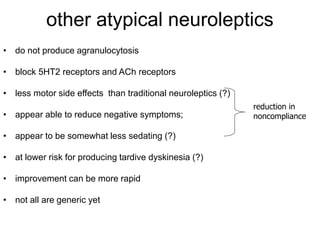
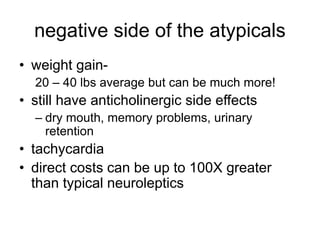
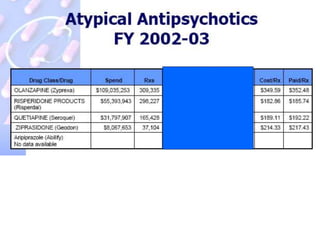
Schizophrenia is characterized by positive and negative symptoms. Positive symptoms include hallucinations while negative symptoms involve a lack of normal behaviors. Traditional neuroleptics effectively treat positive symptoms by blocking dopamine (DA) receptors but have no effect on negative symptoms. Atypical neuroleptics like clozapine are more effective at treating both positive and negative symptoms due to their action on multiple receptor types including serotonin and acetylcholine receptors in addition to DA receptors. However, atypical neuroleptics also carry risks like significant weight gain and metabolic side effects that must be weighed against their benefits.