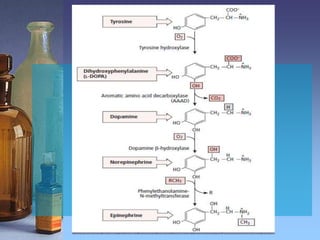
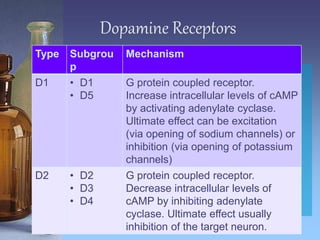
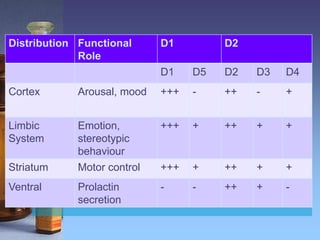
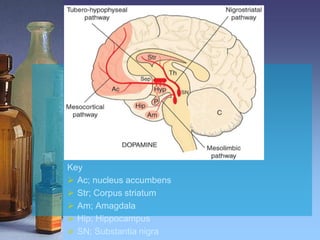
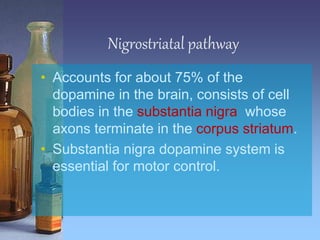
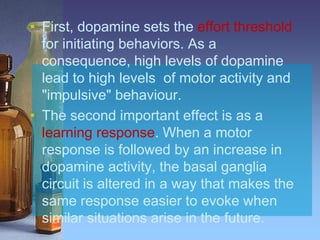
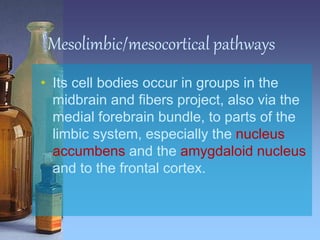
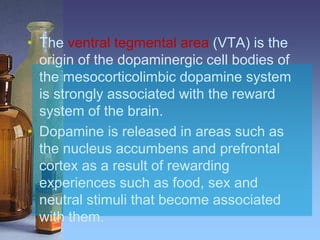
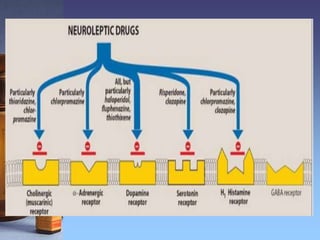
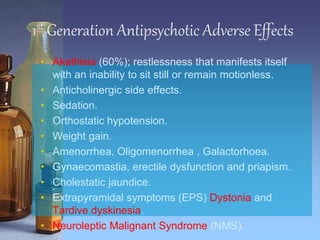
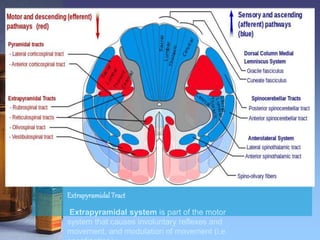
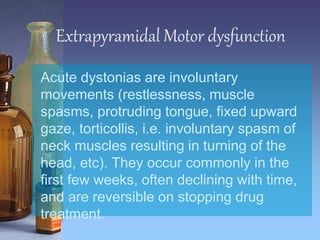
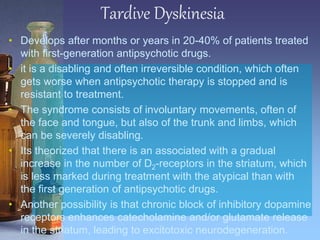
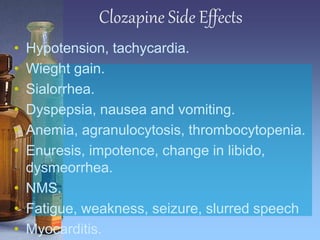
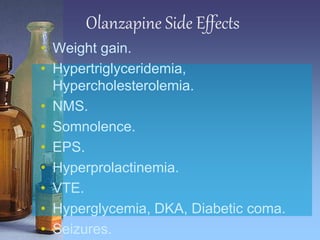
The document provides an overview of antipsychotics, detailing the role of dopamine in the central nervous system and categorizing common antipsychotic medications. It describes the mechanisms of action, side effects, and distinguishes between first-generation (typical) and second-generation (atypical) antipsychotics. Additionally, it covers the implications of dopamine receptor interactions and adverse effects such as extrapyramidal symptoms and neuroleptic malignant syndrome.