This presentation discusses the diagnosis and management of anorectal abscesses. Key points include:
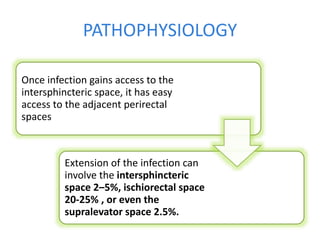
- Anorectal abscesses typically present with perianal pain, swelling, and drainage and are usually caused by a cryptoglandular infection.
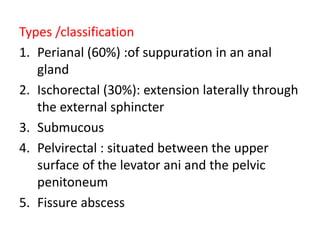
- Differential diagnoses depend on associated symptoms and may include hemorrhoids, fistulas, or Crohn's disease.
- Evaluation involves examination, blood tests, and imaging studies.
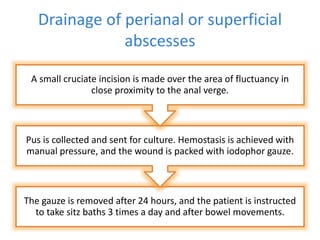
- Treatment is early surgical drainage of the abscess to prevent complications like fistula formation or impairment of sphincter function. Postoperative care involves antibiotics, pain relief, and follow-up to monitor for healing or complications.