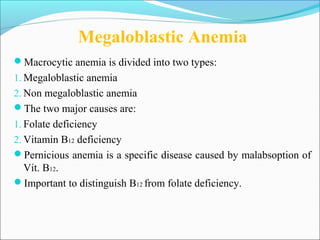
The document discusses vitamin B12 deficiency anemia. It defines anemia and describes the stages and pathophysiology of vitamin B12 deficiency. Key points include:
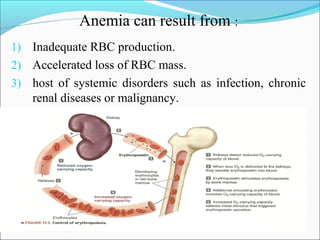
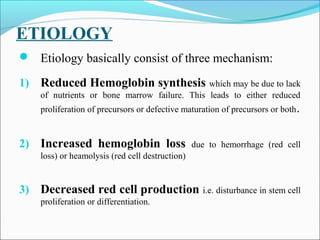
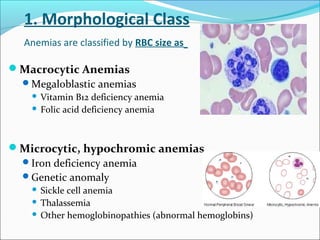
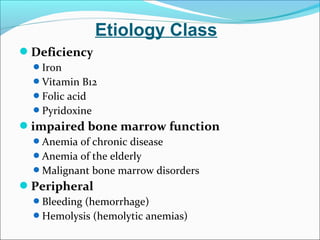
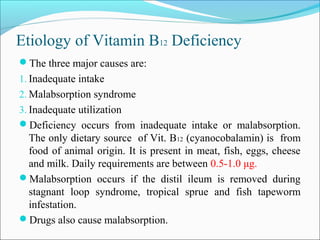
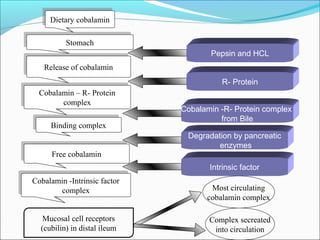
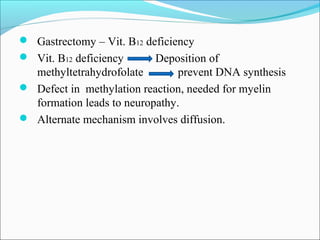
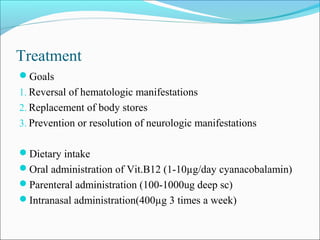
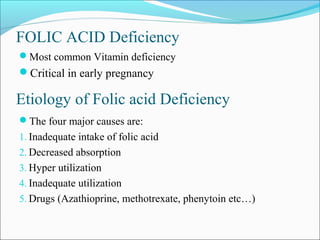
- Vitamin B12 deficiency can result from inadequate intake, malabsorption, or inadequate utilization. The major causes are pernicious anemia resulting from gastric acid and intrinsic factor deficiencies impairing vitamin B12 absorption.
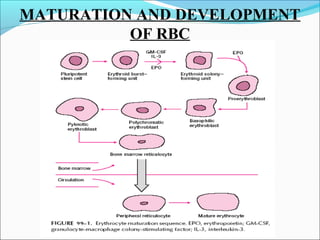
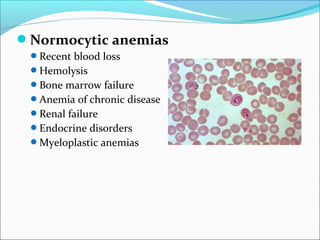
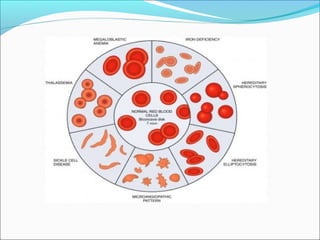
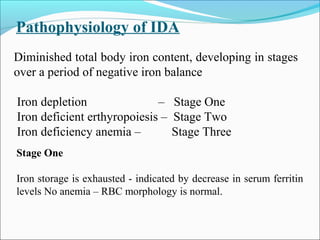
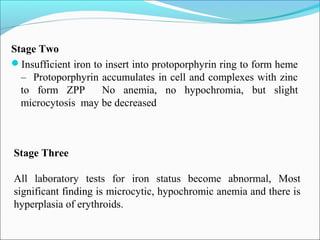
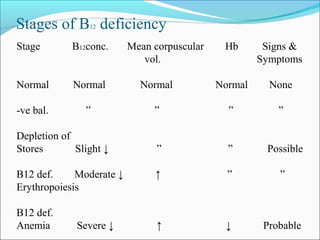
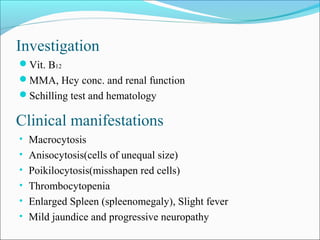
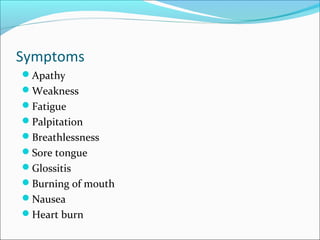
- There are three stages of vitamin B12 deficiency: stores depletion, impaired erythropoiesis, and anemia with neurological symptoms potentially developing at severe deficiency.
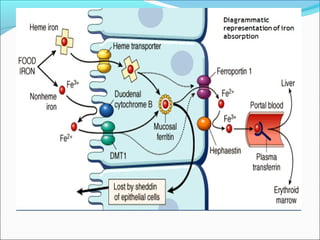
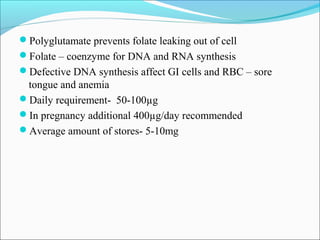
- Vitamin B12 works with folate in DNA/RNA synthesis and its absorption requires intrinsic factor to form a complex for distal ileum absorption. G