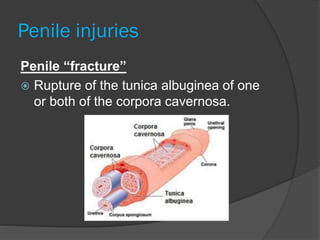
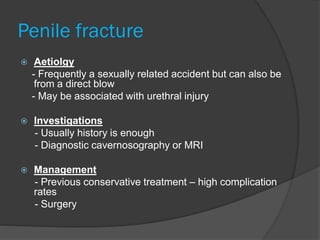
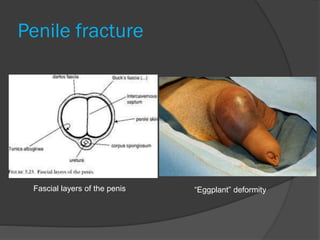
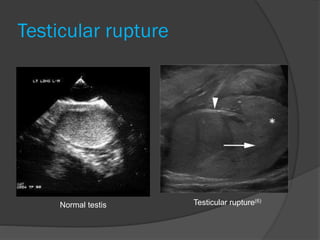
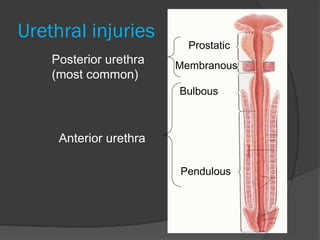
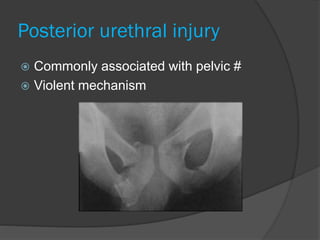
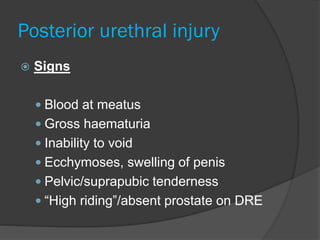
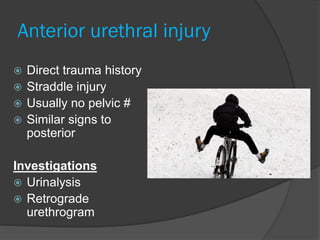
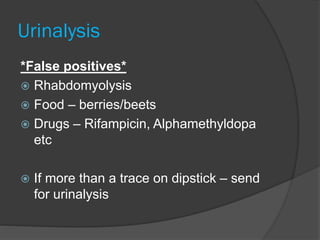
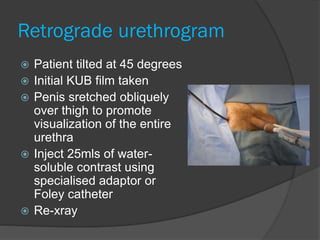
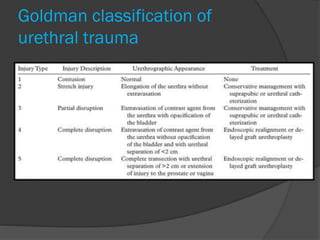
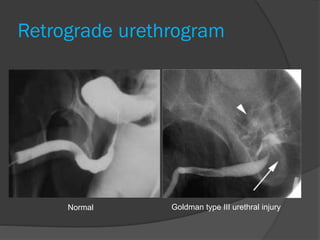
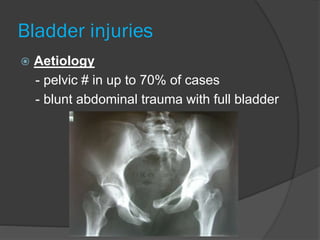
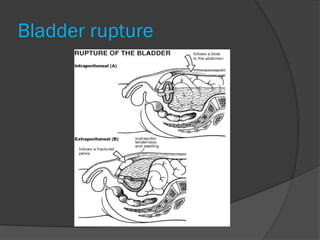
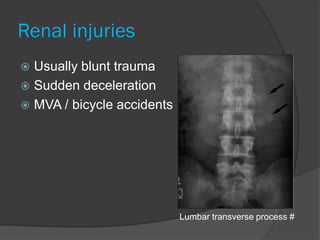
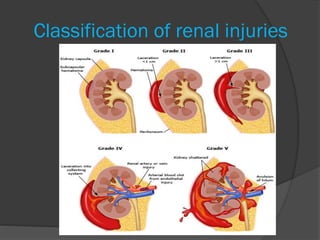
This document provides an overview of genitourinary trauma, including injuries to the penis, testicles, urethra, bladder, ureters and kidneys. It discusses the causes, signs, investigations and management for each type of injury. Penile fractures require surgical repair to prevent long-term complications. Testicular injuries may require ultrasound or surgical exploration. Urethral injuries are classified using the Goldman system and managed conservatively or surgically depending on severity. Bladder injuries often require retrograde cystography and may be managed conservatively or surgically. Renal injuries are graded based on CT or IVP findings and most grade I-II injuries can be managed conservatively while grade III or higher often require