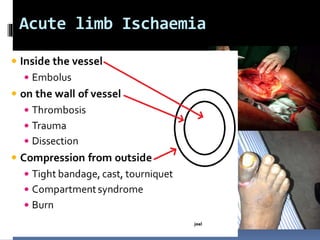
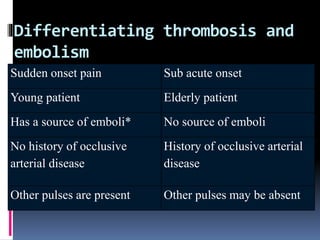
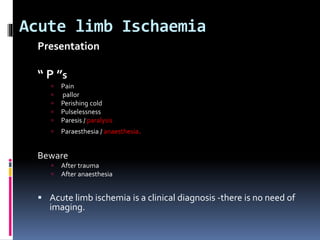
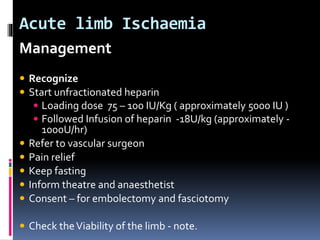
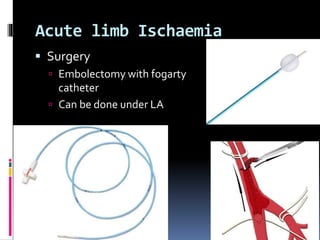
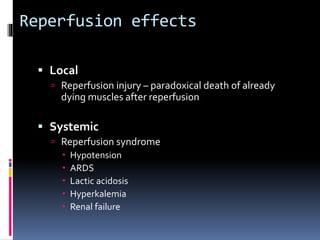
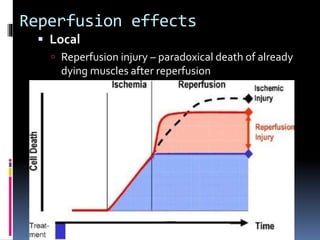
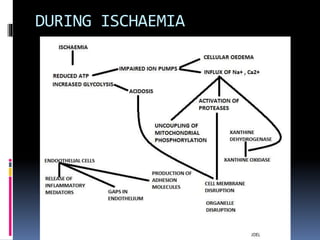
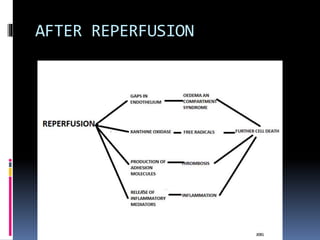
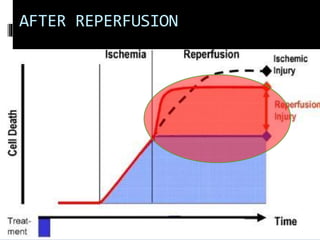
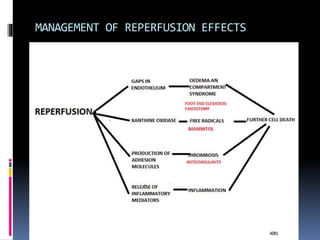
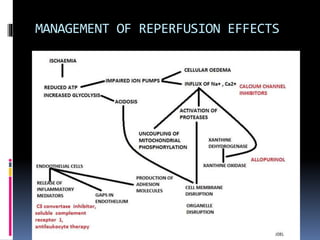
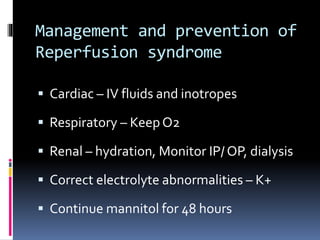
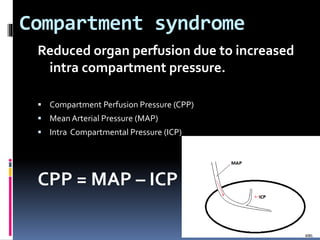
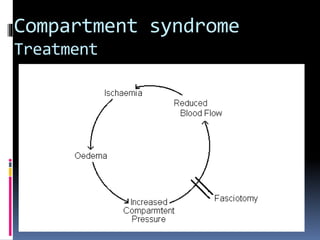
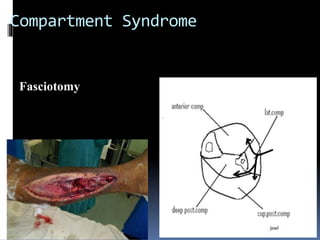
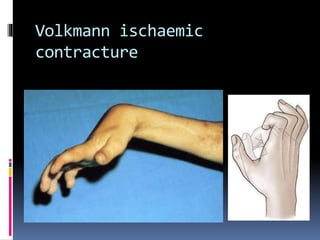
Acute limb ischaemia is a critical condition characterized by a sudden loss of blood supply to a limb, often resulting from thrombosis or embolism. It is diagnosed clinically with symptoms including severe pain, pallor, and pulselessness, and management includes anticoagulation, surgical intervention, and monitoring for complications such as compartment syndrome. Reperfusion effects following treatment can include serious complications like hypotension and lactic acidosis, necessitating careful postoperative management.