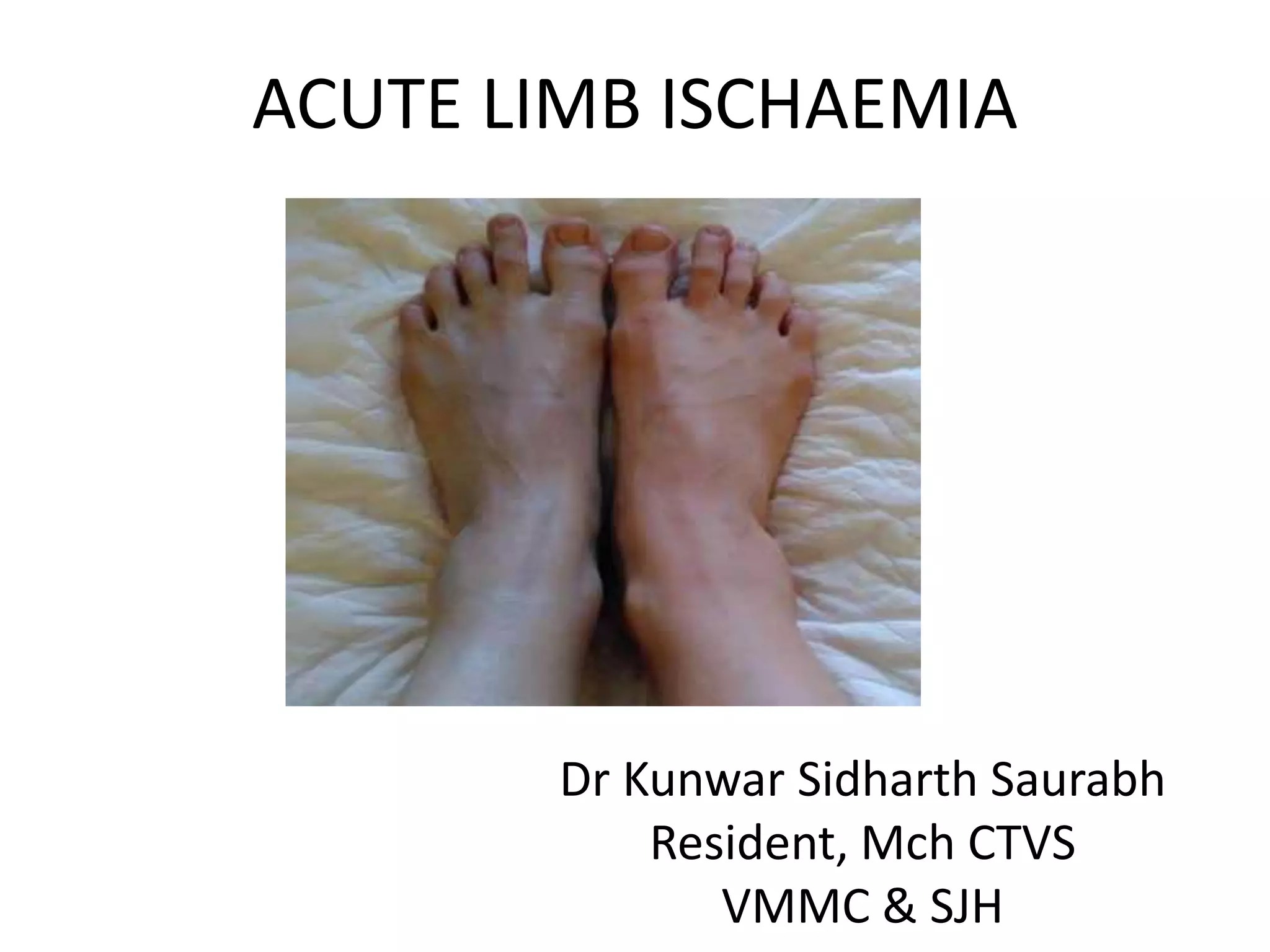
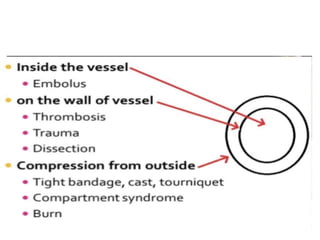
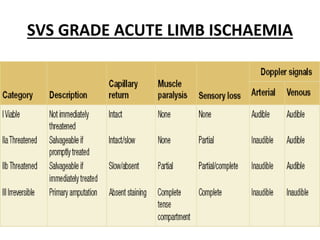
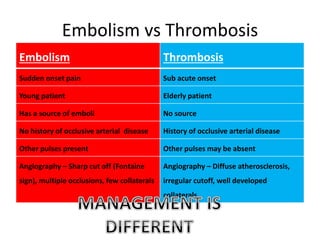
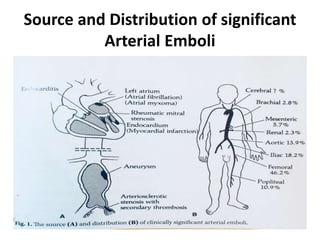
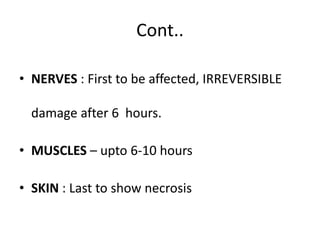
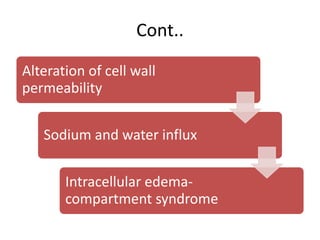
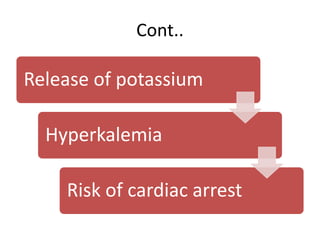
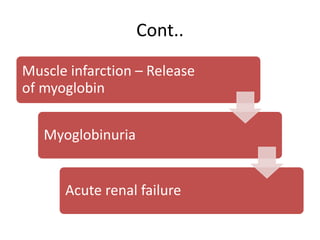
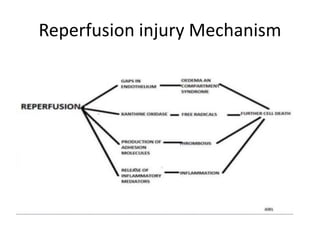
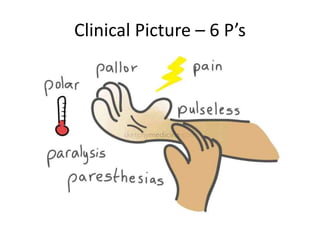
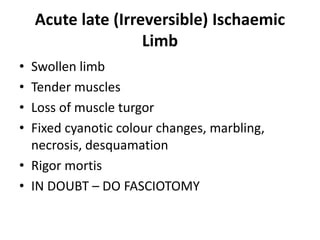
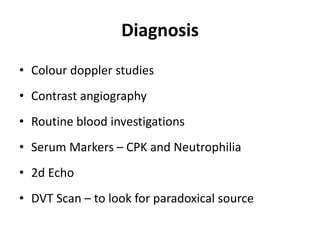
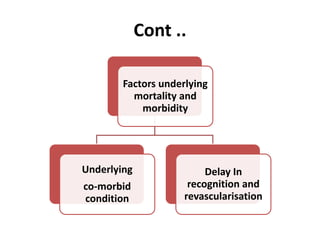
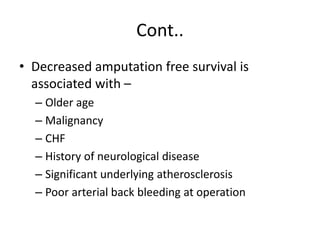
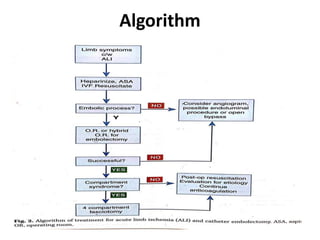
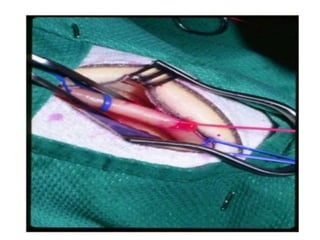
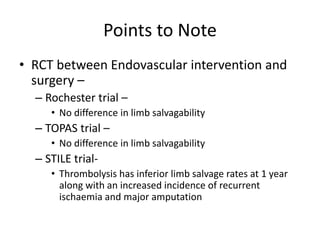
Acute limb ischemia is a vascular emergency defined as a sudden interruption of blood supply to a limb, threatening limb viability. It is commonly caused by arterial embolism or thrombosis. The degree of obstruction, site of occlusion, and presence of collateral circulation determine the pathophysiology. Tissues tolerate ischemia at different rates, with nerves being first affected and skin last. Diagnosis involves imaging studies and blood tests. Treatment depends on whether ischemia is reversible or irreversible, with anticoagulation, endovascular intervention, open surgery, or amputation used depending on the situation. Factors like delay in treatment and underlying conditions impact outcomes.