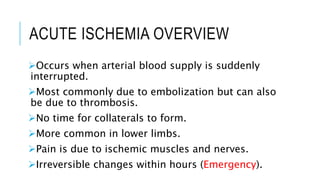
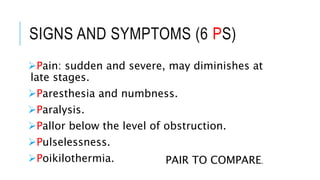
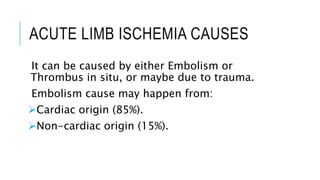
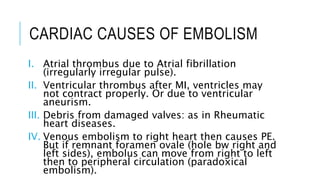
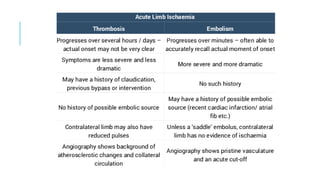
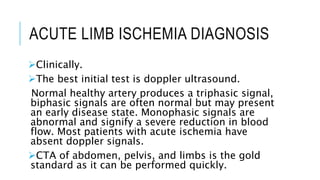
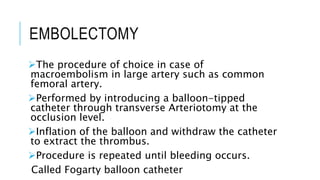
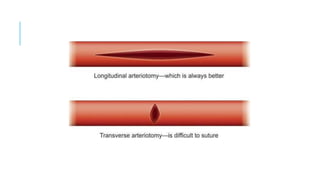
The document discusses acute ischemia and compartment syndrome. Acute ischemia occurs when blood supply is suddenly interrupted, most commonly due to embolism or thrombosis. It can cause severe pain and irreversible tissue damage within hours. Treatment depends on the severity and includes heparin, hydration, embolectomy, and thrombolysis. Compartment syndrome is a painful emergency condition caused by increased pressure within a muscle compartment, blocking blood flow. It requires early fasciotomy to decompress the compartment if diagnosed in the first 8 hours.