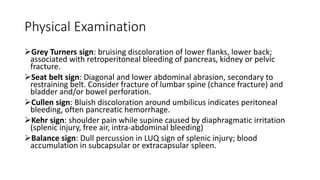
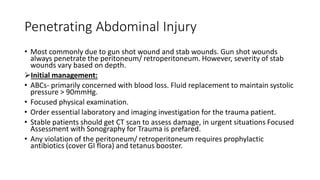
The document provides an overview of abdominal trauma, categorizing it into blunt and penetrating injuries, detailing the common organs affected and their clinical features. It outlines initial management principles, including resuscitation, diagnostics, and indications for exploratory surgery, along with specific notes on managing injuries to organs such as the liver and spleen. Additionally, it discusses complications associated with abdominal trauma and emphasizes the importance of timely intervention and proper evaluation.