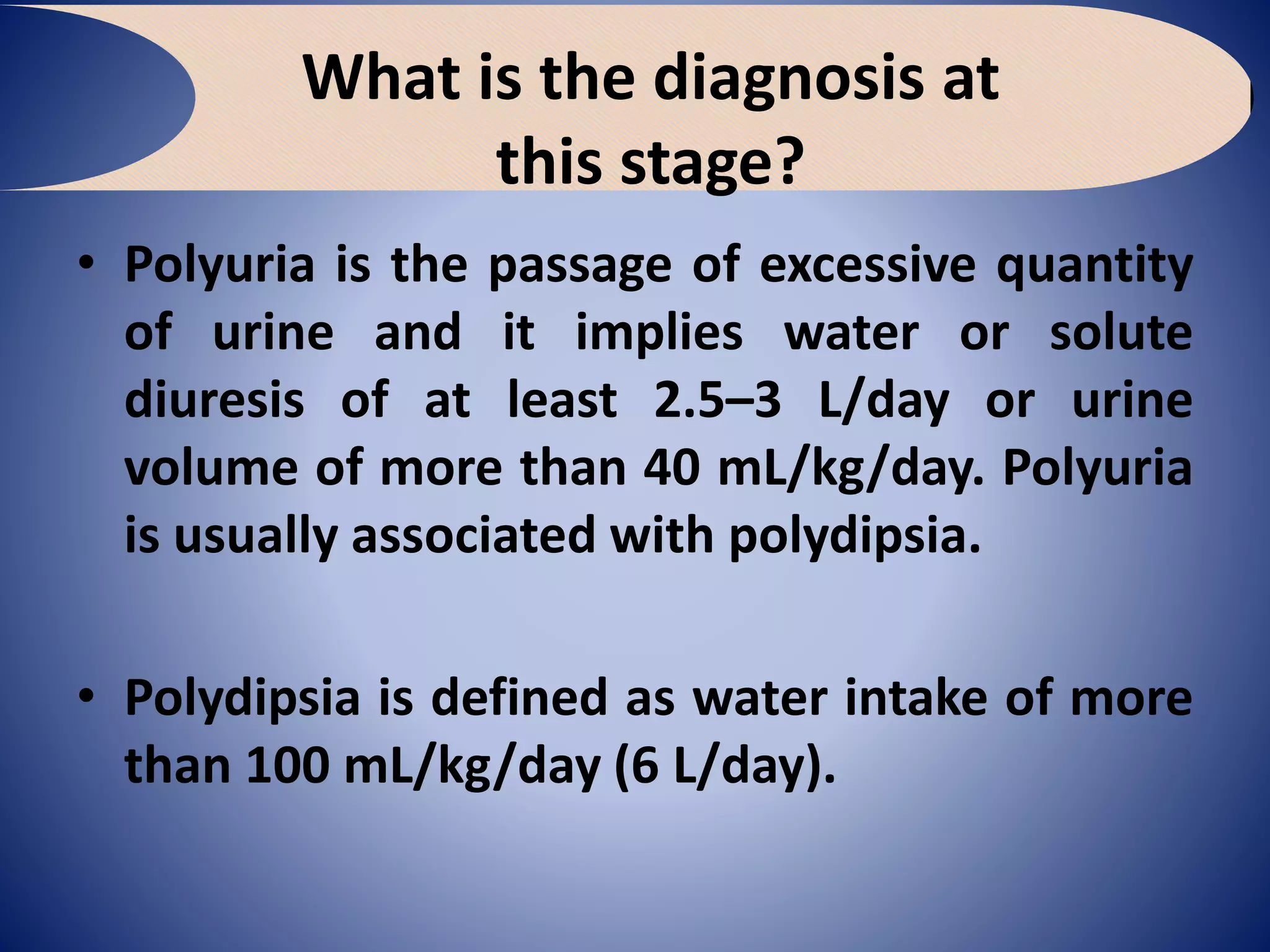
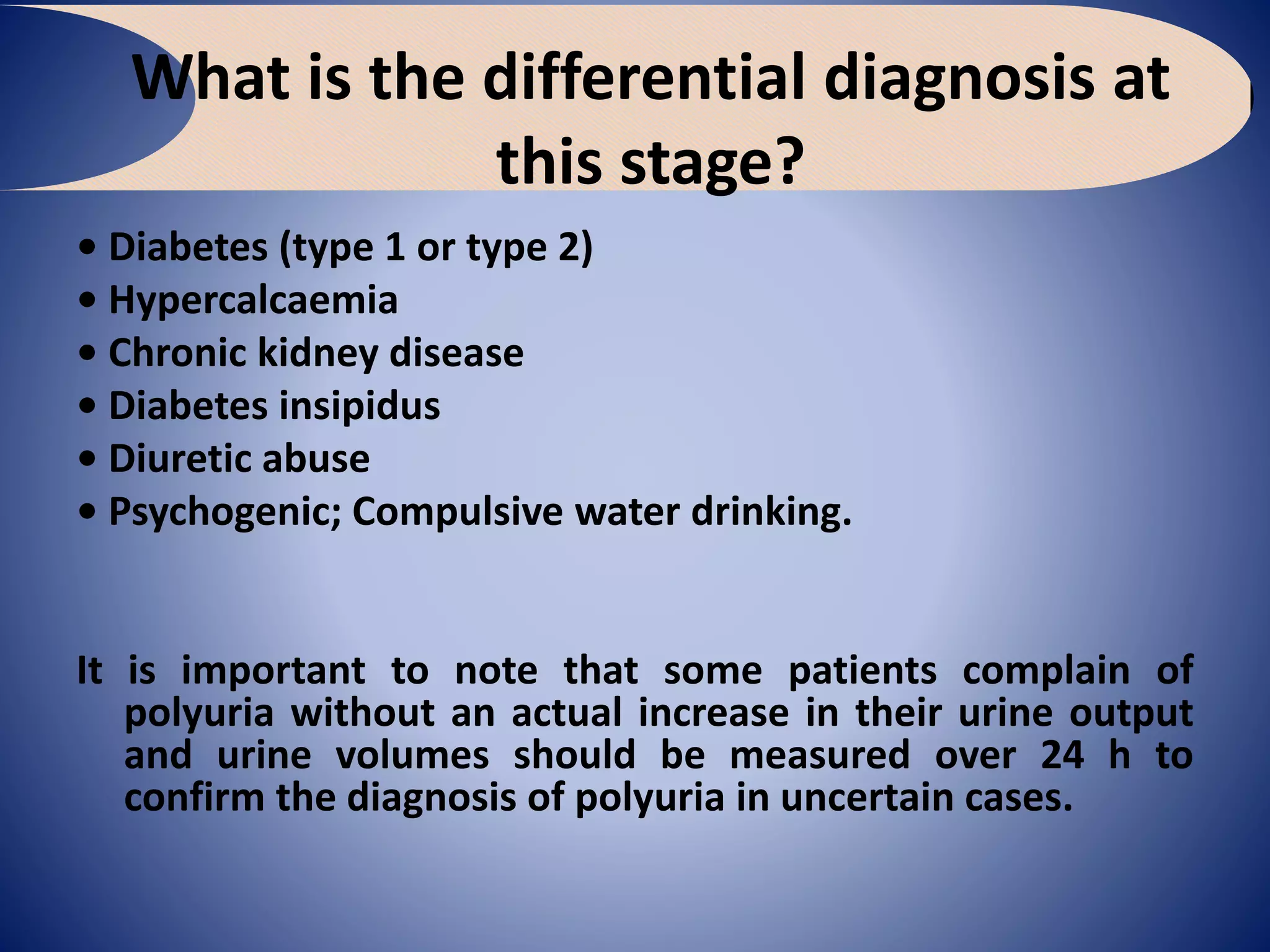
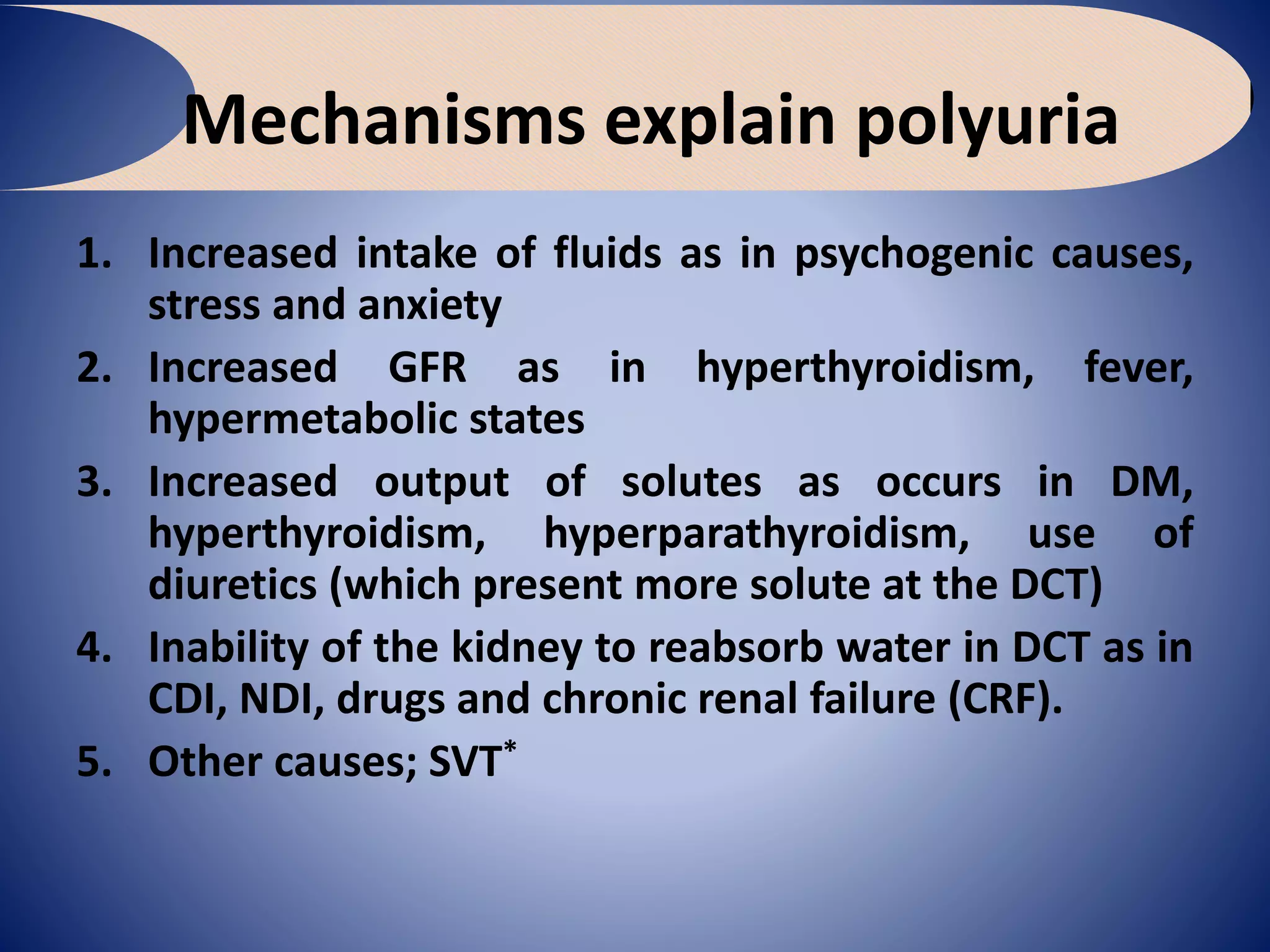
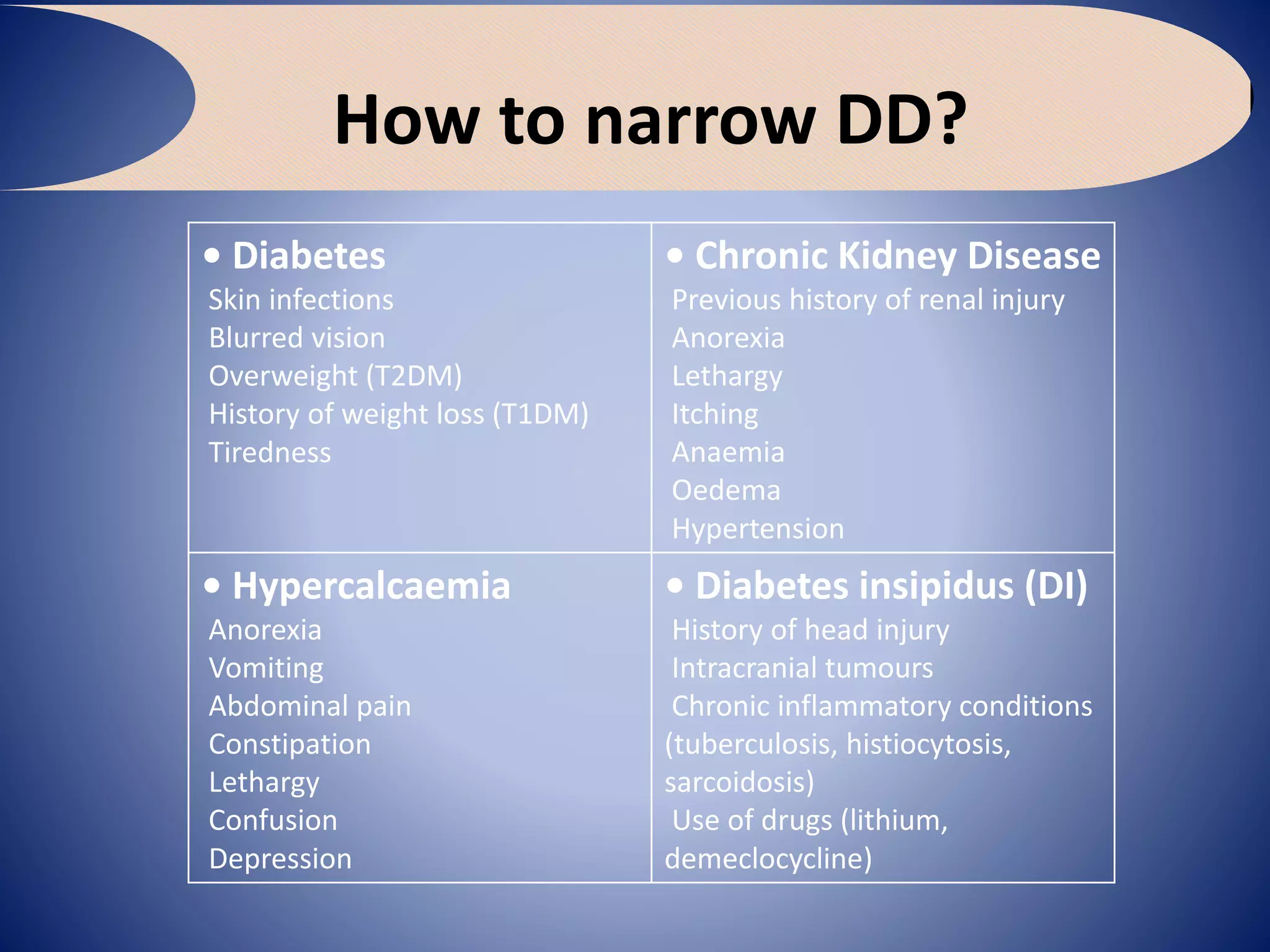
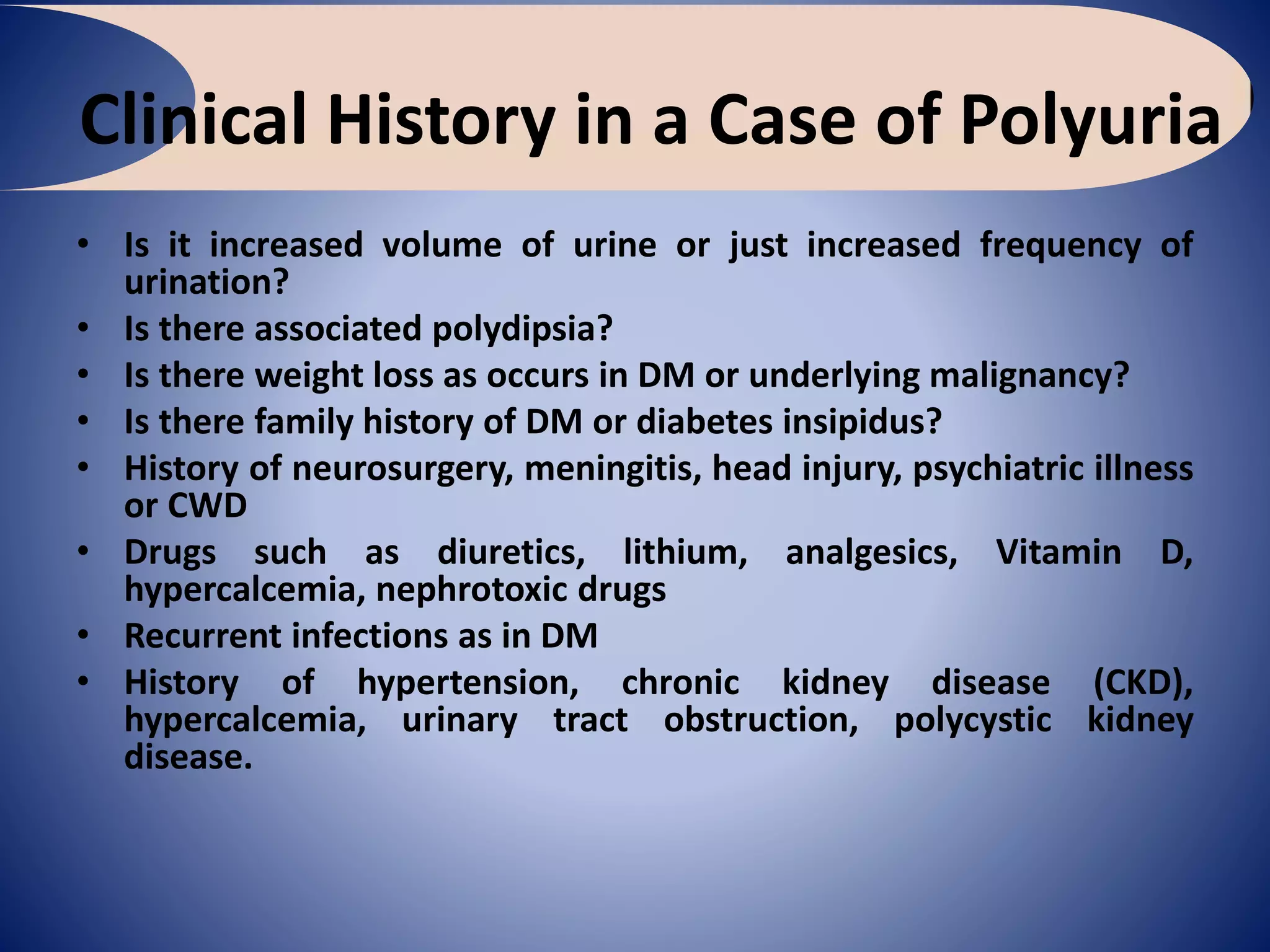
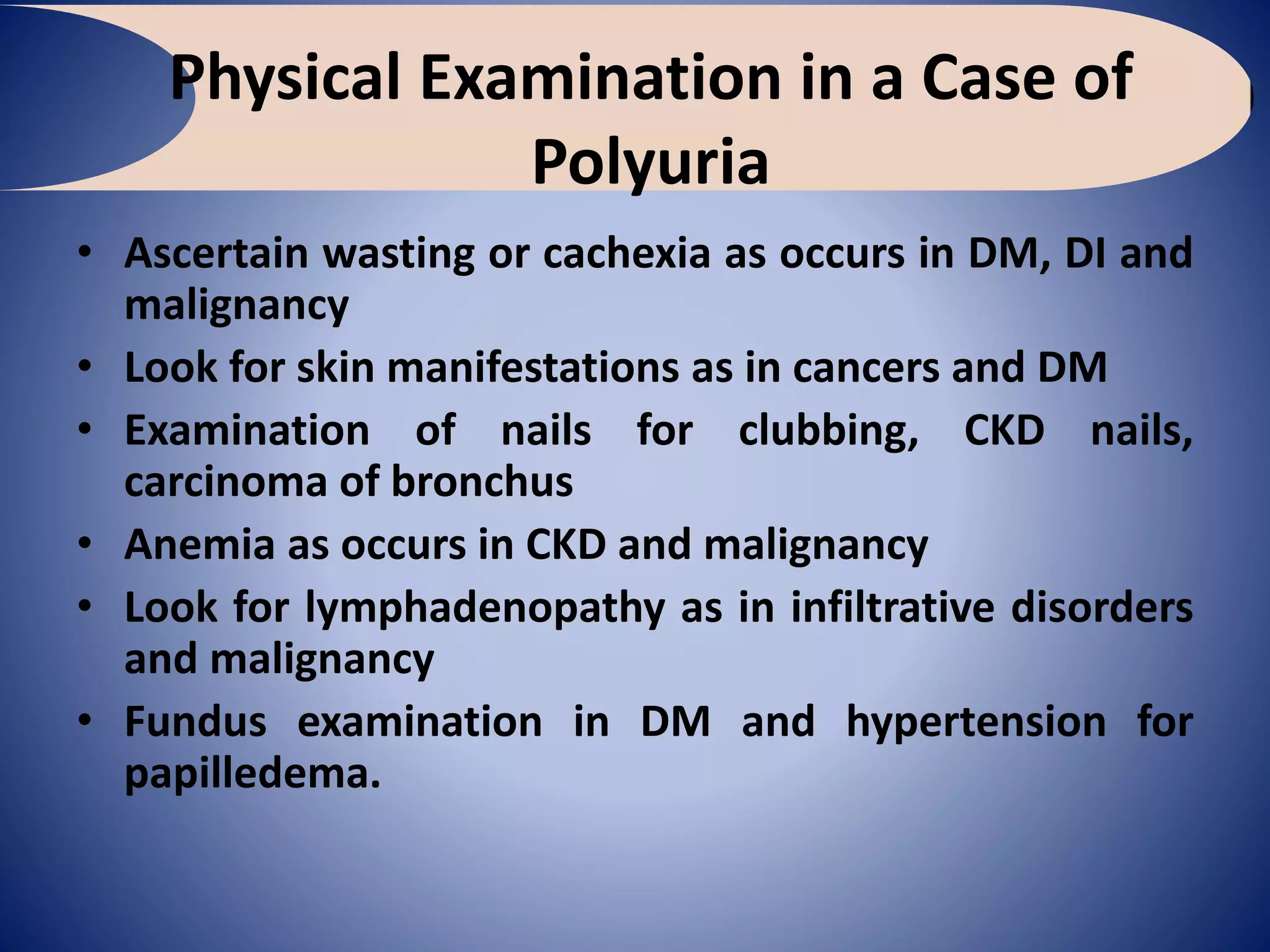
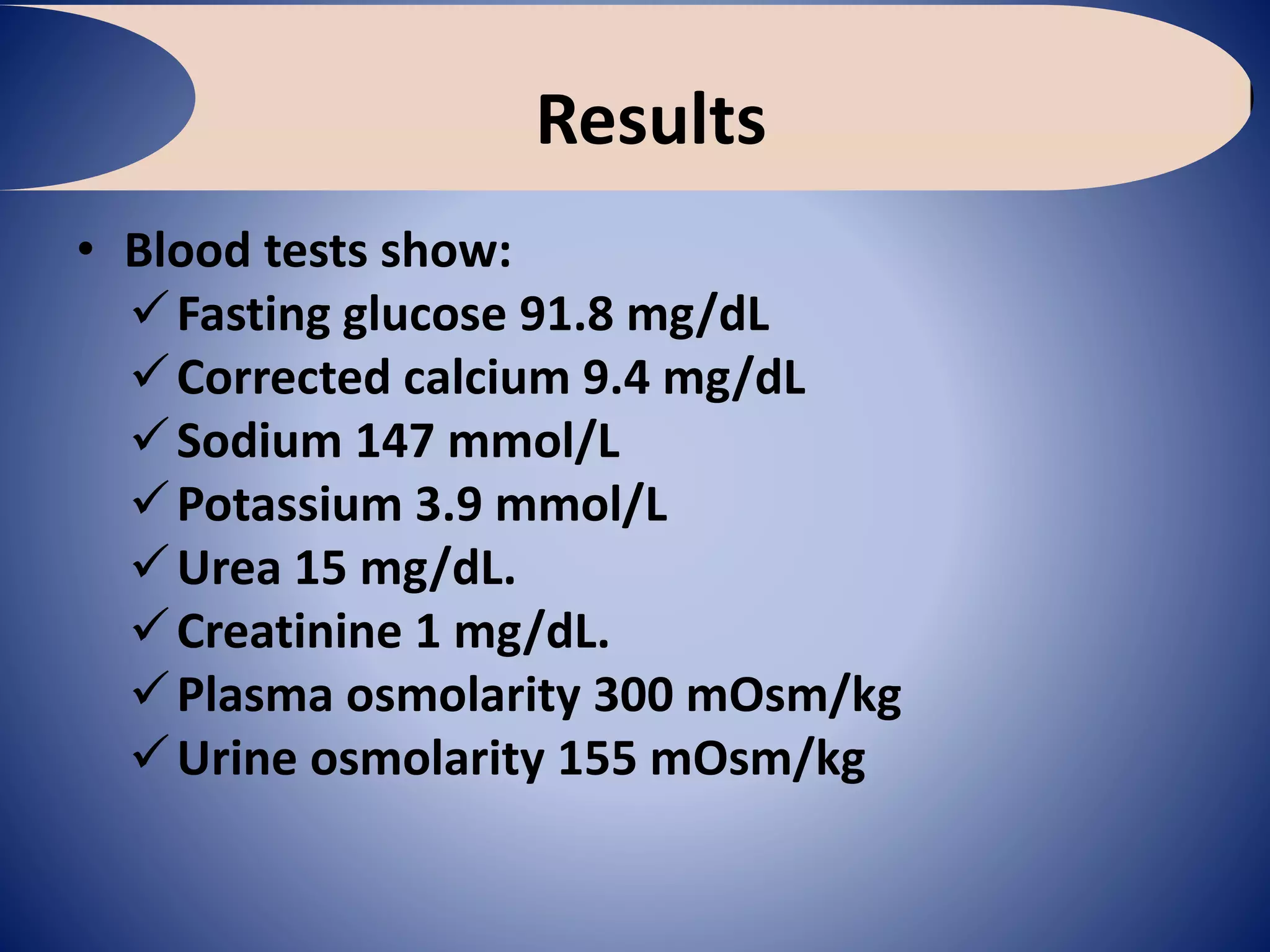
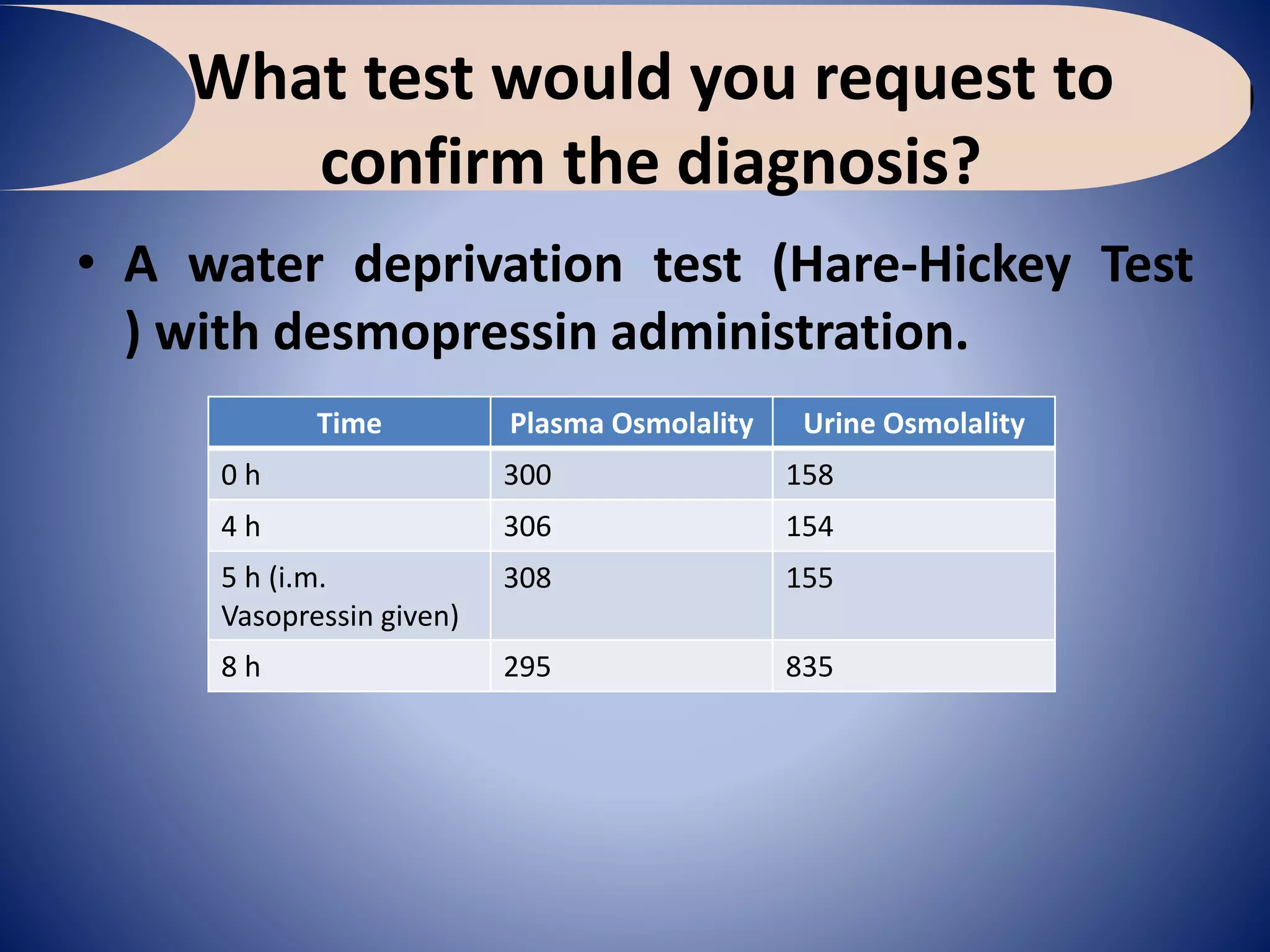
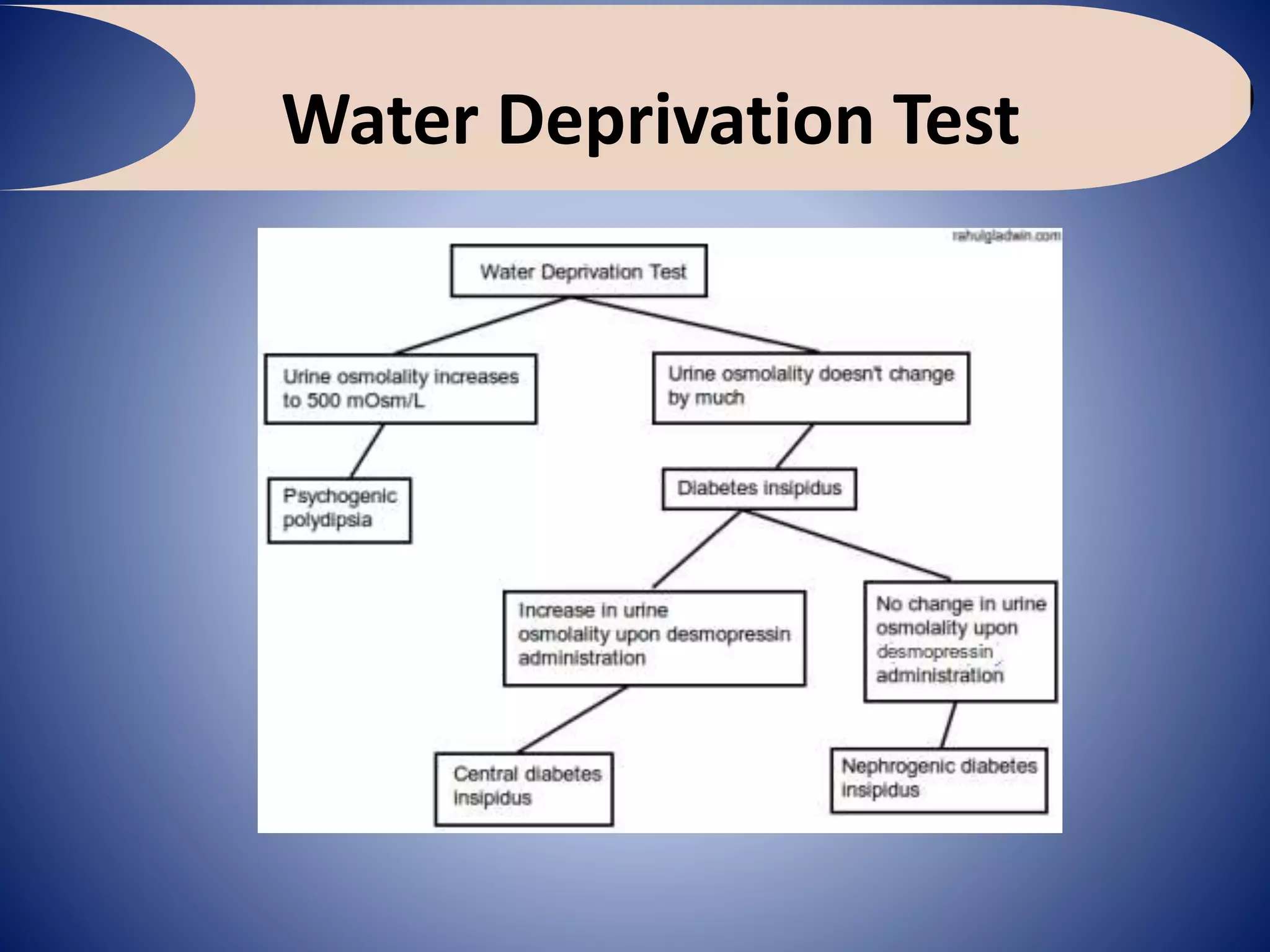
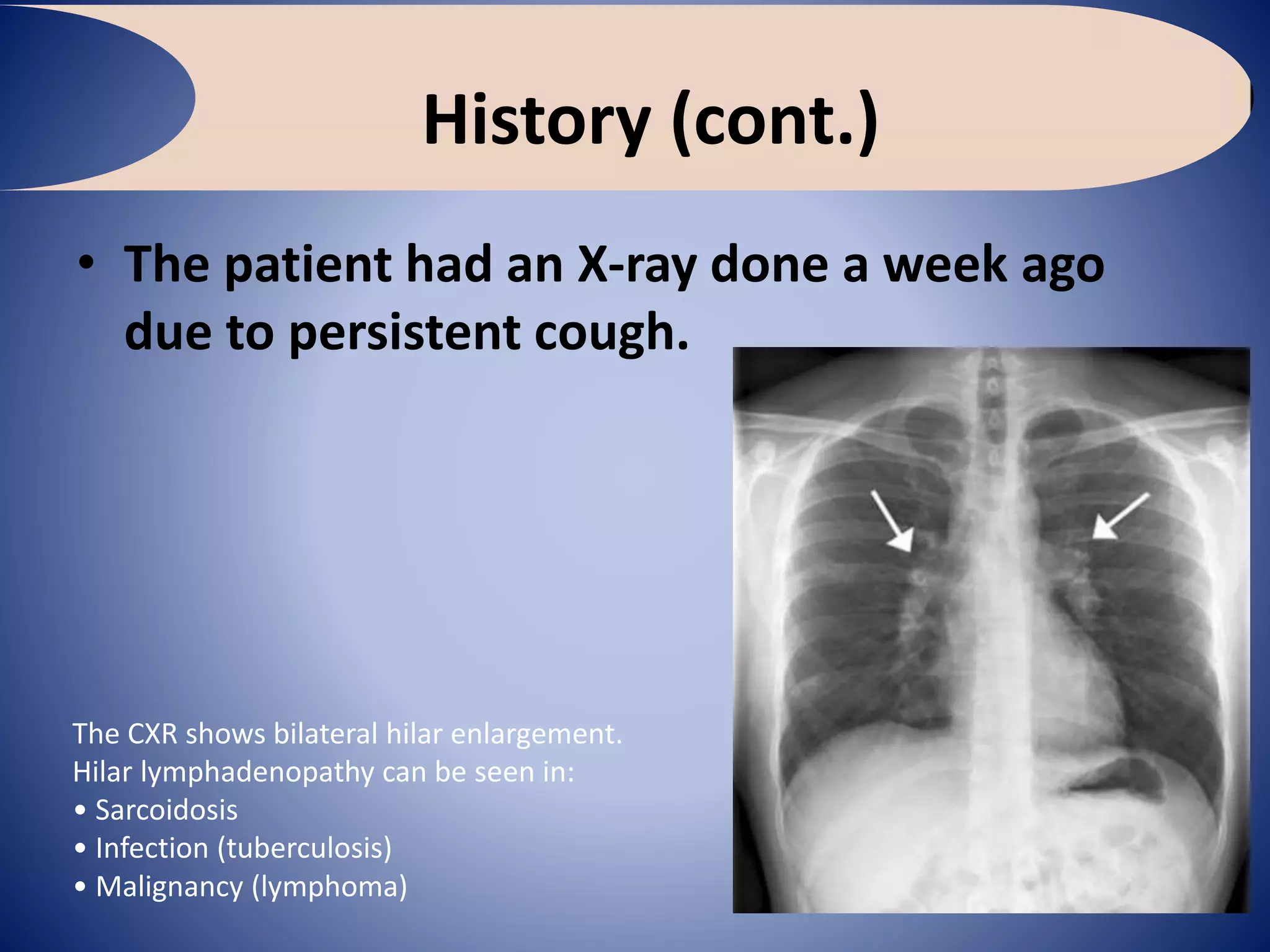
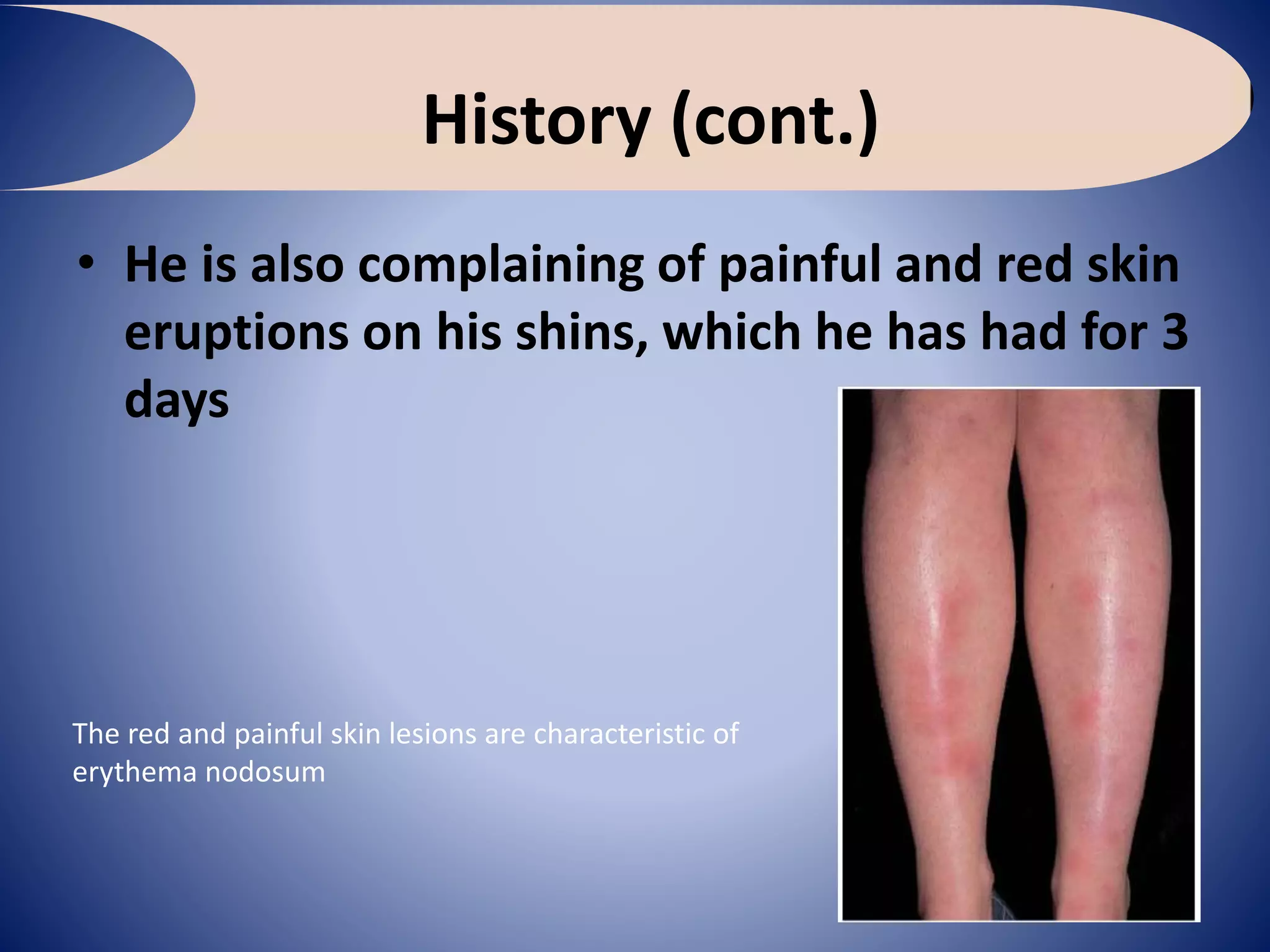
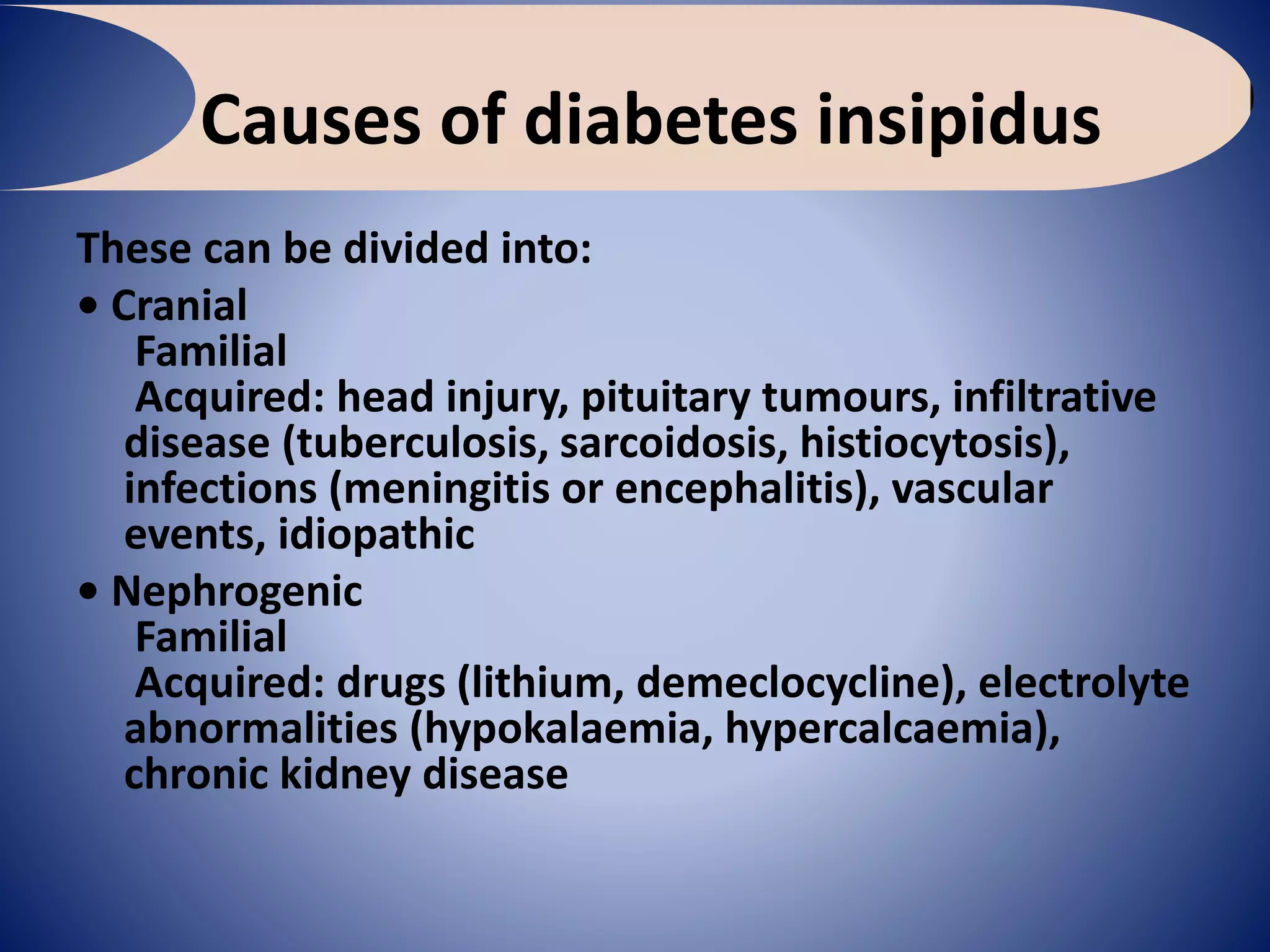
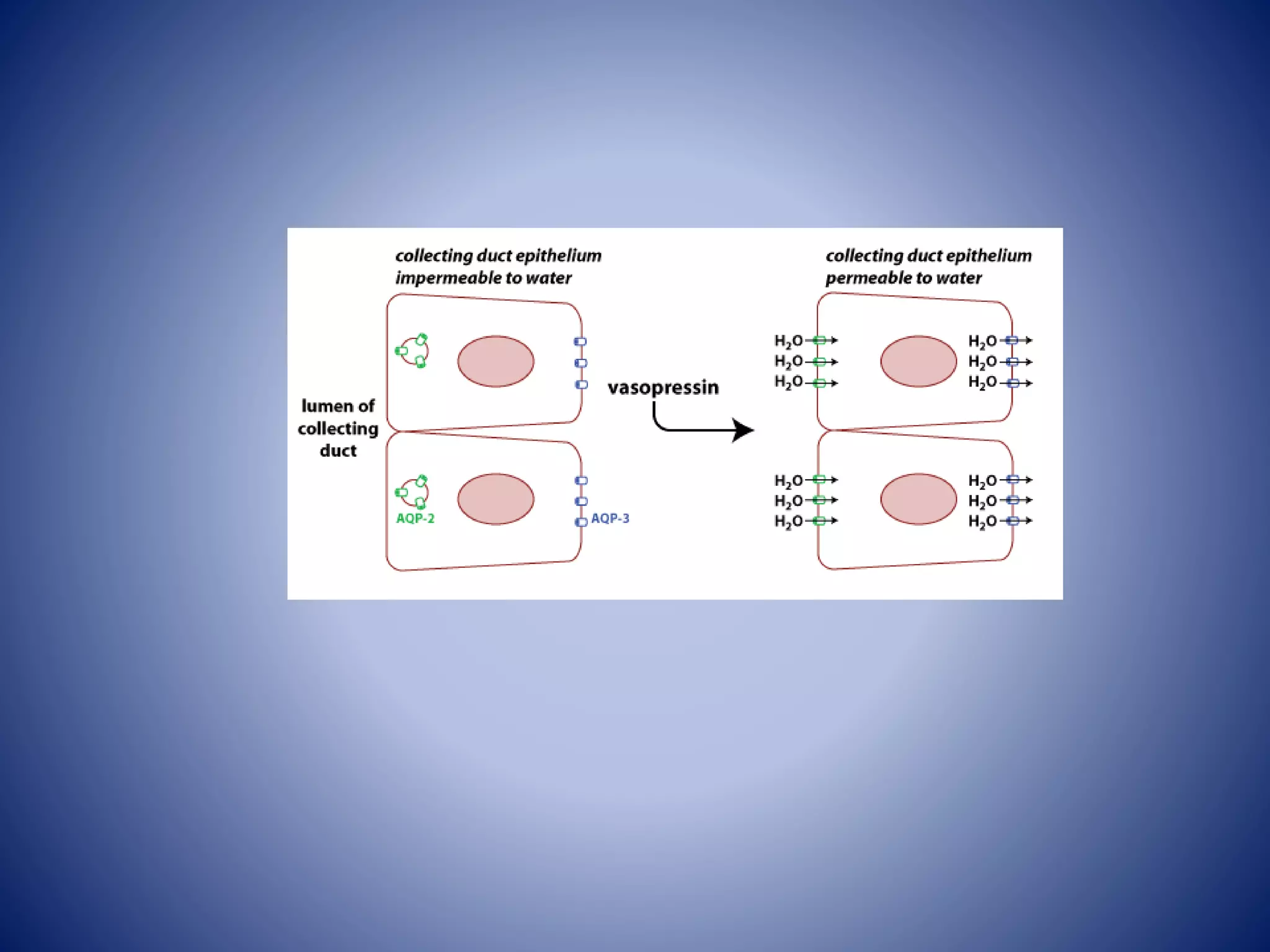
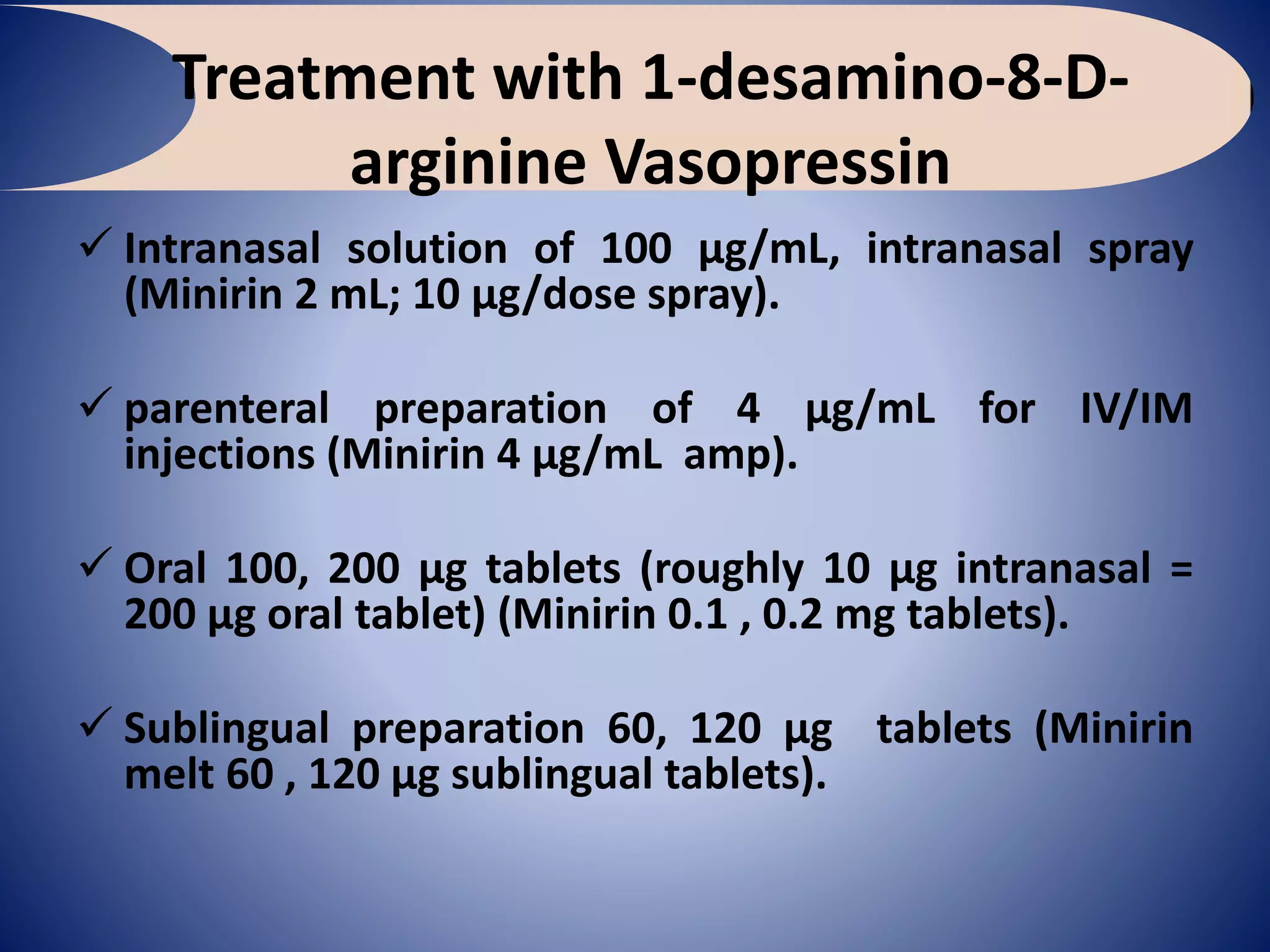
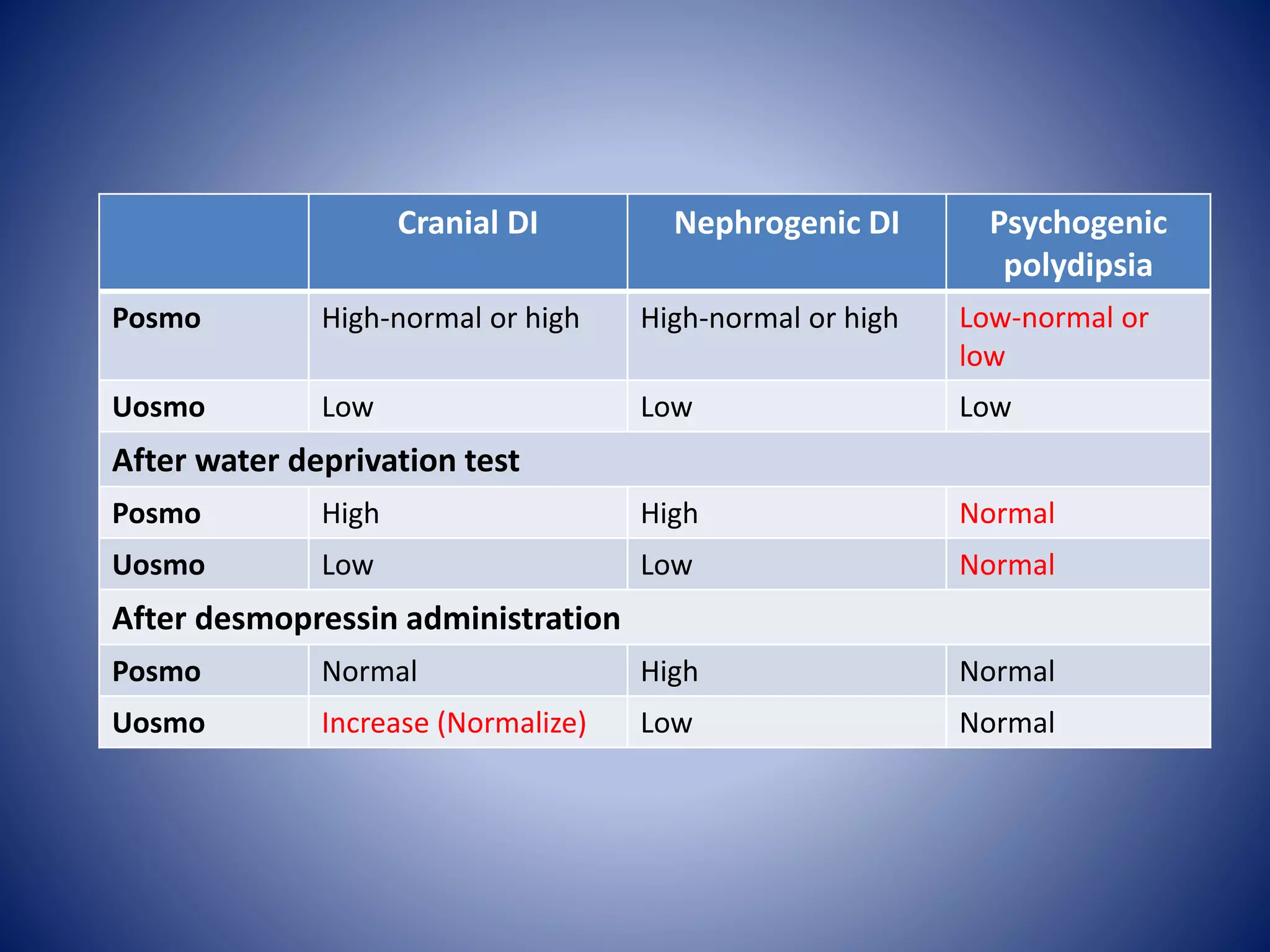
A 33-year-old man named Peter is experiencing polyuria and polydipsia, ultimately diagnosed with diabetes insipidus (DI) after a water deprivation test. His symptoms are linked to sarcoidosis as indicated by abnormal chest X-ray findings and skin lesions consistent with erythema nodosum. Treatment for DI involves the administration of desmopressin, which can be given in various forms.