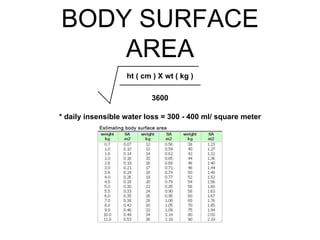
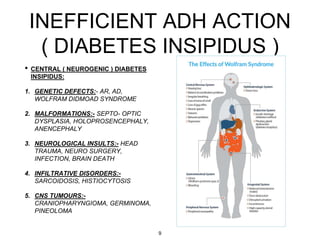
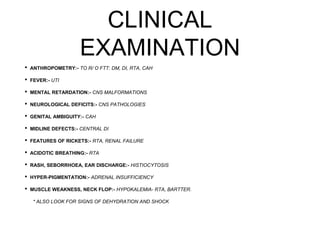
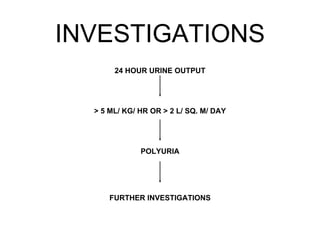
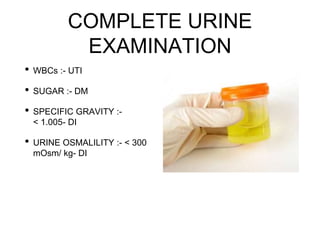
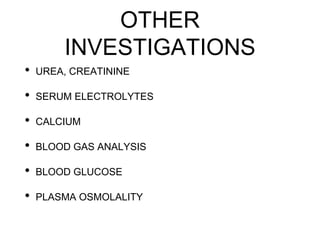
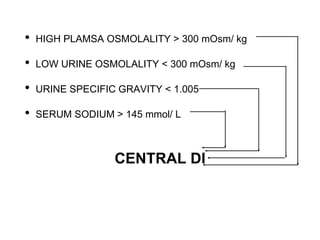
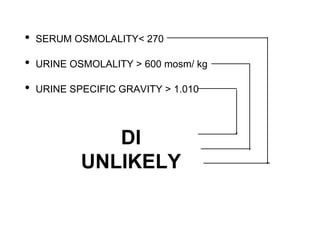
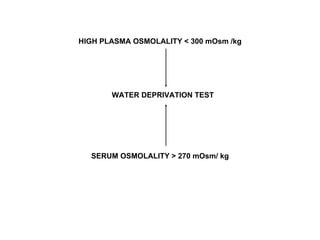
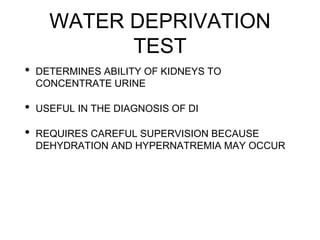
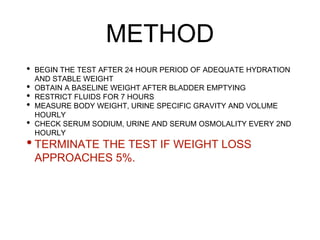
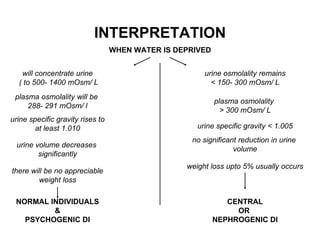
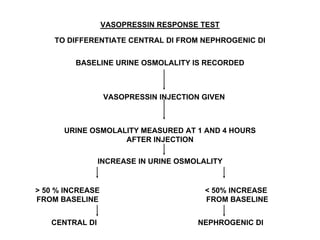
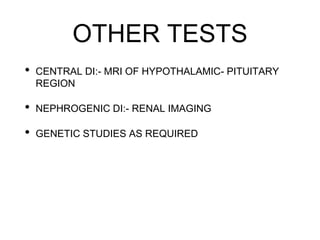
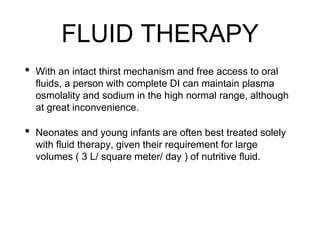
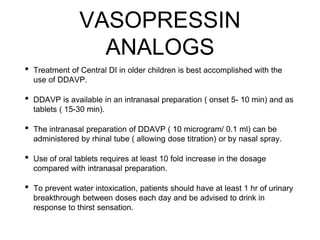
This document discusses the approach to polyuria, defined as urine output greater than 5 mL/kg/hr or 2 L/m2/day. It outlines the main causes of polyuria as increased fluid intake, increased urinary solute excretion, or impaired urinary concentration. The approach involves obtaining a history, clinical examination, and investigations including a 24-hour urine output and further tests based on initial findings. Treatment depends on the underlying cause, and may include fluid therapy, vasopressin analogs for central diabetes insipidus, or reducing the underlying disorder and limiting fluid intake for nephrogenic diabetes insipidus.