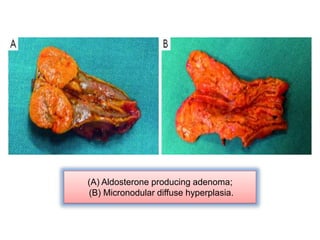
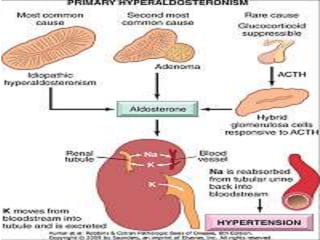
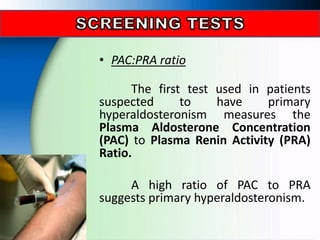
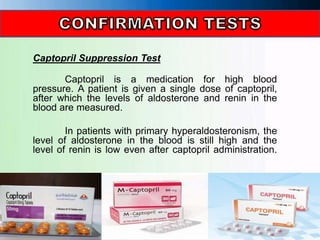
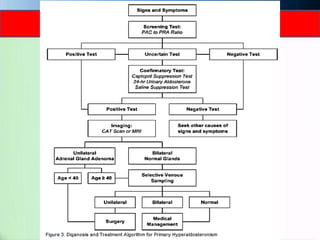
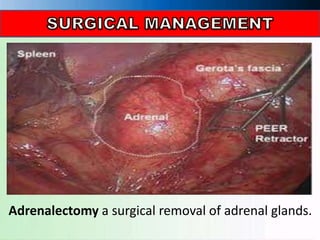
Primary aldosteronism is caused by excessive secretion of the hormone aldosterone from the adrenal glands. This can be due to an aldosterone-producing adenoma or adrenal hyperplasia. Symptoms include hypertension, hypokalemia, muscle weakness, and fatigue. Tests used to diagnose include the PAC/PRA ratio, captopril suppression test, saline suppression test, and CT scan. Treatment options are mineralocorticoid receptor antagonists, surgery to remove the adrenal glands, and lifestyle changes like reducing sodium intake. Management involves monitoring blood pressure and electrolyte levels.