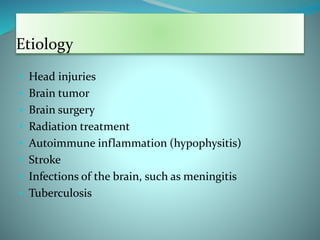
A 22-year-old university student presents with symptoms of excessive thirst, drinking 20-25 glasses of water per day and waking up 5-6 times per night to pass urine. She is constipated but has a normal appetite and weight. The differential diagnoses are psychogenic polydipsia, diabetes mellitus, and diabetes insipidus. Diabetes insipidus is defined as the excretion of large volumes of dilute urine and can be central or nephrogenic in origin. Central diabetes insipidus results from a decreased secretion of antidiuretic hormone due to conditions affecting the hypothalamus or pituitary gland.