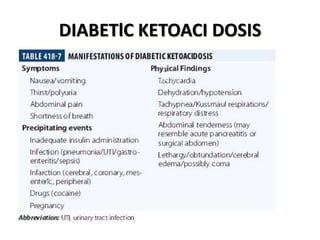
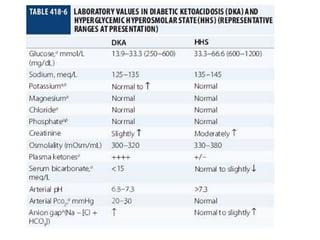
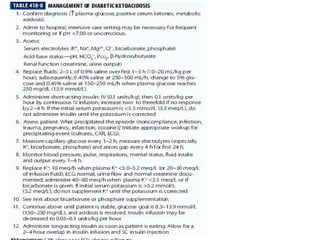
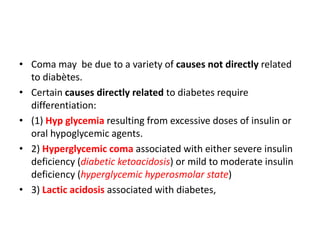
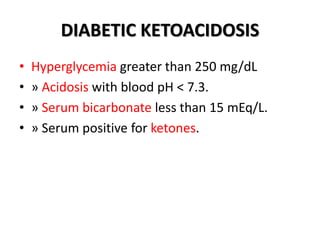
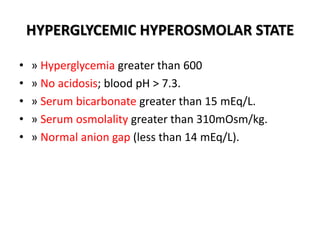
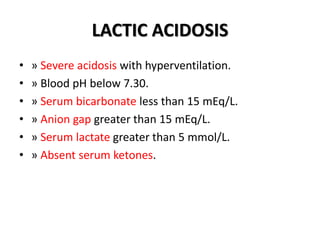
The document discusses different types of diabetic comas including hypoglycemic coma, diabetic ketoacidosis, hyperglycemic hyperosmolar state, and lactic acidosis. It provides diagnostic criteria for each condition including specific ranges for blood pH, serum bicarbonate, ketones, glucose, osmolality, and anion gap. Diabetic ketoacidosis is associated with severe insulin deficiency and hyperglycemia over 250 mg/dL while hyperglycemic hyperosmolar state involves hyperglycemia over 600 mg/dL without acidosis. Lactic acidosis presents with severe acidosis, elevated lactate, and absent ketones.
![Hyperglycemic coma
• Individuals with type 1 or type 2 DM and severe
hyperglycemia [300 mg/dL] ) should be assessed for
clinical stability; including mentation and hydration.
• the patient is stable or if diabetic ketoacidosis or a
hyperglycemic hyperosmolar state should be
considered.
• Ketones,an indicator of diabetic ketoacidosis,
should be measured in individuals with type 1 DM
when the plasm glucose is > (300 mg/dL) , during a
concurrent illness, or with symptoms such as
nausea, vomiting, or abdominal pain.
• Blood measurement of ß-ydroxybutarrate is
preferred over urine](https://image.slidesharecdn.com/diabeticcoma-181108040020/85/Diabetic-coma-6-320.jpg)