Bladder carcinoma is a prevalent urologic cancer, primarily comprising transitional cell carcinoma (TCC), with a notable male-to-female ratio and varying prognoses across races. Significant predisposing factors include environmental exposures, chronic inflammation, and genetic mutations, while clinical presentation often features hematuria and irritative urinary symptoms. Treatment approaches involve surgery, chemotherapy, and immunotherapy, tailored according to tumor stage and patient condition.

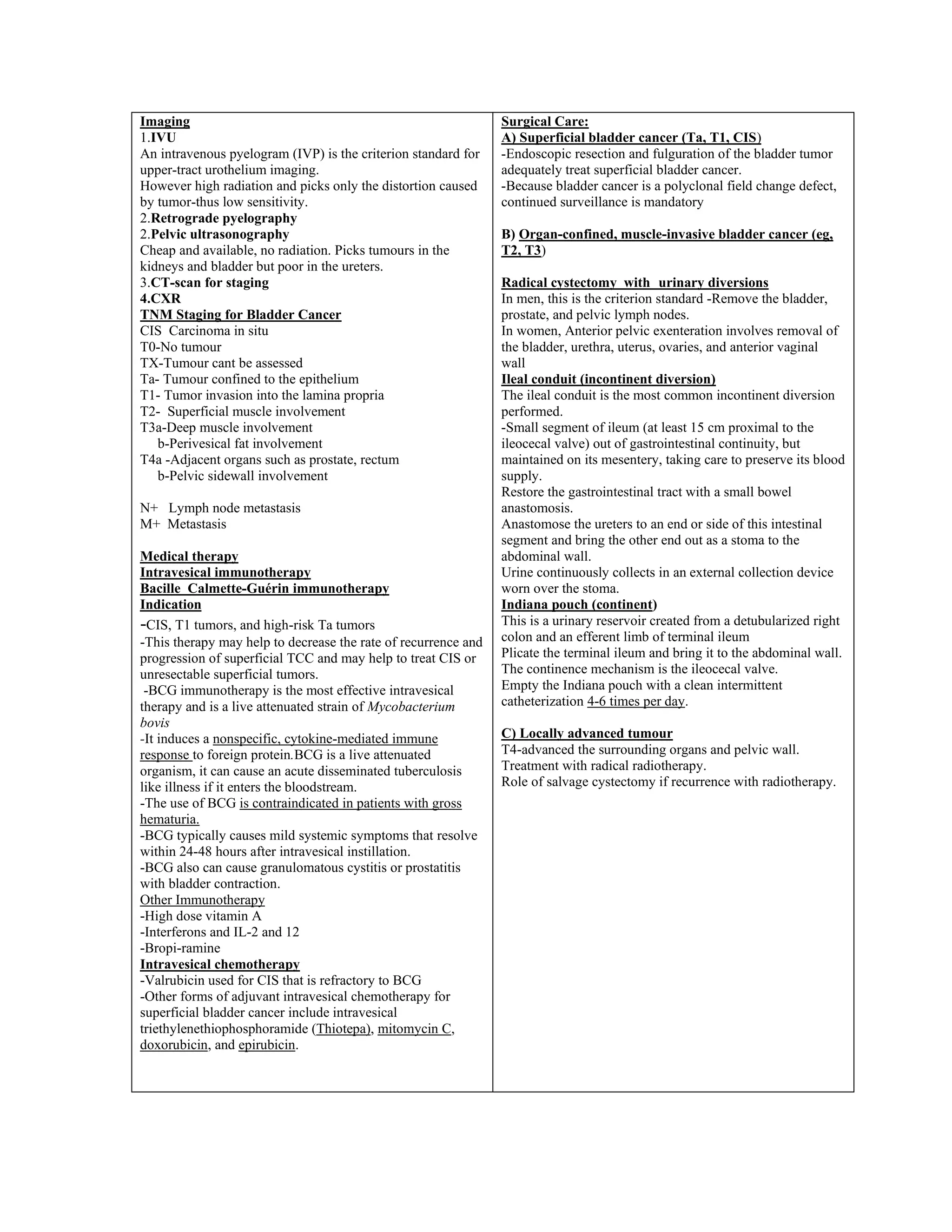
![BLADDER CARCINOMA
Introduction
-Bladder cancer is a common urologic cancer.
-4th
most common tumour in men after lung, prostate and
colorectal cancer.
-Most cases are transitional cell carcinoma (TCC)
worldwide, often described as polyclonal field change
defects. In Kenya the TCC and SCC are thought to be about
50% each.
-Urothelium in the entire urinary tract may be involved,
including the renal pelvis, ureter, bladder, and urethra.
-Nonurothelial primary bladder tumors are rare and may
include
1) Rhabdomyosarcoma
2) Small cell carcinoma
3) Carcinosarcoma
4) Sarcoma
5) Primary lymphoma
Sex and Age
-The male-to-female ratio is 3:1.
-Women generally have a worse prognosis than men.
-The median age at diagnosis is 68 years, and the incidence
increases directly with age
Race:
-Bladder cancer is more common in whites than blacks;
however, blacks have a worse prognosis
Pathophysiology:
Predisposing factors below.
-Adenocarcinomas account for less than 2% of primary
bladder tumors.
-These tumors are observed most commonly in exstrophic
bladders and are poorly responsive to radiation and
chemotherapy. Radical cystectomy is the treatment of
choice. Also develop in persistent urachus.
-Most squamous cell carcinomas of the bladder in are
associated with persistent inflammations from
1) Chronic cystitis-schistosomiasis
2) Long-term indwelling Foley catheters
3) Bladder stones.
-Small cell carcinomas are thought to arise from
neuroendocrine stem cells and are aggressive tumors that
carry a poor prognosis.
-Carcinosarcomas are highly malignant tumors that contain
both mesenchymal and epithelial elements.
-Primary bladder lymphomas arise in the submucosa of the
bladder and are treated with radiation therapy.
Leiomyosarcoma is the most common sarcoma of the
bladder.
Rhabdomyosarcomas most commonly occur in children and
carry a poor prognosis
Predisposing factors :Environmental
1. Cigarette Smoking-Nitrosamine, 2-naphthylamine, and 4-
aminobiphenyl are possible carcinogenic agents
2.Industrial exposure to aromatic amines in dyes, paints,
solvents, leather dust, inks, combustion products, rubber, and
textiles
3.Prior radiation treatments to the pelvis
4. Exposure to acrolein, a urinary metabolite of
cyclophosphamide, increases the risk of bladder cancer.
5.Artificial sweeteners (eg, saccharin, cyclamate)
SCC
1)chronic cystitis-schistosomiasis
2)long-term indwelling Foley catheters
3)bladder stone
Genetic
1. Mutations of the tumor suppressor gene p53, found on
chromosome 17 and Rb gene in chromosome 13.
2. Mutations of the tumor suppressor genes p15 and p16,
found on chromosome 9.
Clinical presentation
History
1. Painless global hematuria mostly gross hematuria but may
be microscopic
2.Irritative symptoms-dysuria, frequency, urgency
3.Obstructive symptoms especially around the bladder neck.-
poor stream, straining, incomplete emptying
4.Passage of tissue particles
5.Mucosuria-Adenocarcinoma
6.Renal failure signs -oedema
-Inquiry of signs of advanced disease
➢ Back pains
➢ Hematochizia
➢ Pain on defecation
-Any other bleeding from rest of the body
-.Inquiry of predisposing factors-above
Physical examination
Clinical examination is usually normal, although an
abdominal or pelvic mass may be palpable in those with
advanced disease.
Anemia -hematuria
DDX-Causes of heamaturaia
1.Hemorrhagic Cystitis: Noninfectious
2.Nephrolithiasis
3.Renal Cell Carcinoma
4.Transitional Cell Carcinoma, Renal
5.Ureteral Trauma
6.UTI
Investigations
1.FHG-Hb-Anaemia,WBC-UTI, Platelates-Hemorrhage
2.Urinalysis-Nitrites-UTI
Microscopy-Microscopic hematuria.In surgical hematuria
the RBC are not dysmorphic but in medical RBC may
appear dysmorphic.
3.Urine cytology -for malignant cells
4.U/E/C- Upper tract involvement
5.Tumour markers
-Bladder tumor antigen [BTA-Stat]
-Nuclear matrix protein [NMP-22]
-Fibrin/fibrinogen degradation products [FDP])
-Telomerase
6. Flexible cystoscopy
-Urine for cytology
-Biopsy of the areas with lesions or just sampled biopsy.
-Resection of superficial tumors.
Chemotherapy for metastatic cancer
-The Methotrexate, Vinblastine, Adriamycin, and Cisplatin
(M-VAC) or (MAC-V ) combination is the standard
treatment of metastatic bladder cancer.](https://image.slidesharecdn.com/bladdercarcinoma-221121164128-e65f501a/75/BLADDER-CARCINOMA-pdf-2-2048.jpg)