Urinary Bladder Tumor
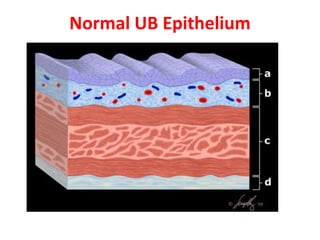
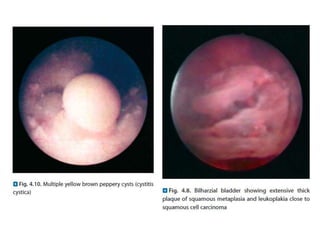
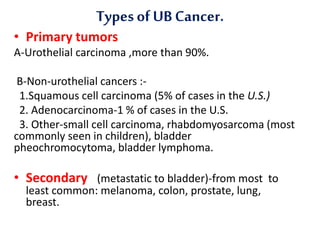
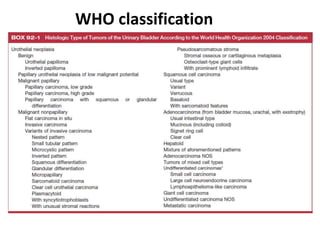
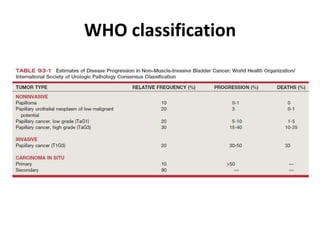
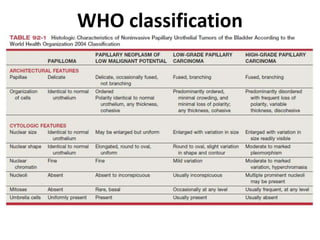
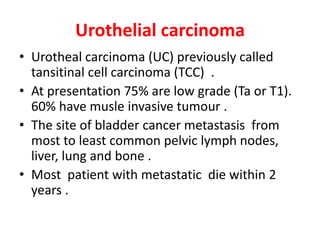
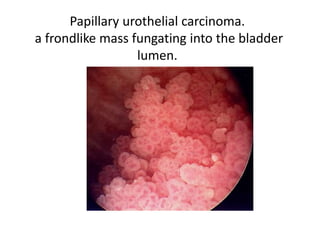
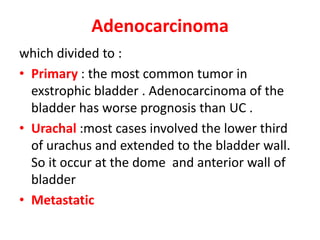
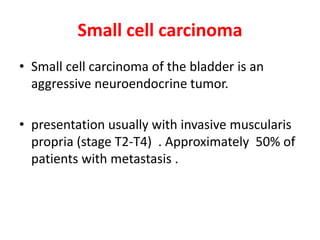
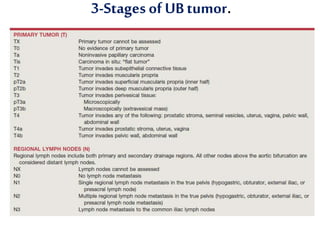
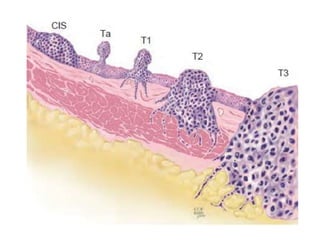
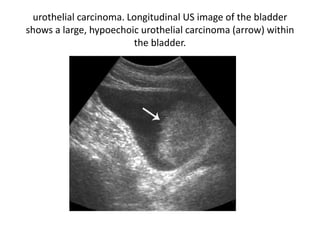
The document discusses urinary bladder tumors. It covers the incidence, risk factors, signs and symptoms, types and classification, staging, and radiological findings of bladder tumors. Bladder cancer is the second most common urological malignancy and is more common in men than women. Major risk factors include smoking and occupational exposure to carcinogens. Common presenting symptoms are painless visible blood in the urine and recurrent urinary tract infections. Types include urothelial carcinoma (90% of cases), squamous cell carcinoma, and adenocarcinoma. Staging uses the TNM system. Radiological exams like ultrasound, CT, and MRI can identify bladder tumors and their extent.