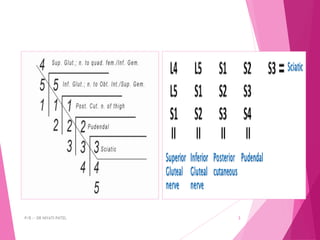
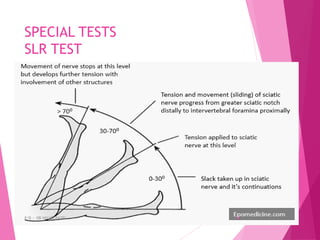
This document discusses sciatic neuropathy, including its anatomy, causes, signs and symptoms, investigations, types of injuries, and treatments. The sciatic nerve is the thickest nerve in the body and originates from the lumbosacral plexus, supplying muscles in the lower limb. Causes of sciatic neuropathy include pelvic fractures, hip dislocations, and compression by tumors. Signs include sensory loss and muscle paralysis below the knee, resulting in foot drop and gait abnormalities. Investigations include MRI, EMG, and nerve conduction studies. Treatments focus on preventing contractures and foot drop through electrical stimulation, splinting, and customized footwear.