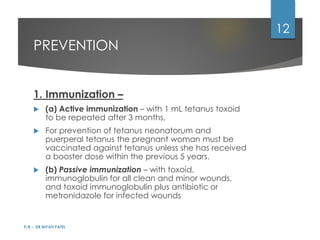
Tetanus is caused by a neurotoxin produced by Clostridium tetani bacteria that enters the body through wounds or burns. It causes muscle spasms by blocking motor neuron synapses in the central nervous system. Symptoms range from lockjaw to generalized painful muscle spasms. Treatment involves wound care, antibiotics, medications to control spasms, and supportive care like ventilation for severe cases. Prevention centers on immunization and proper wound management.