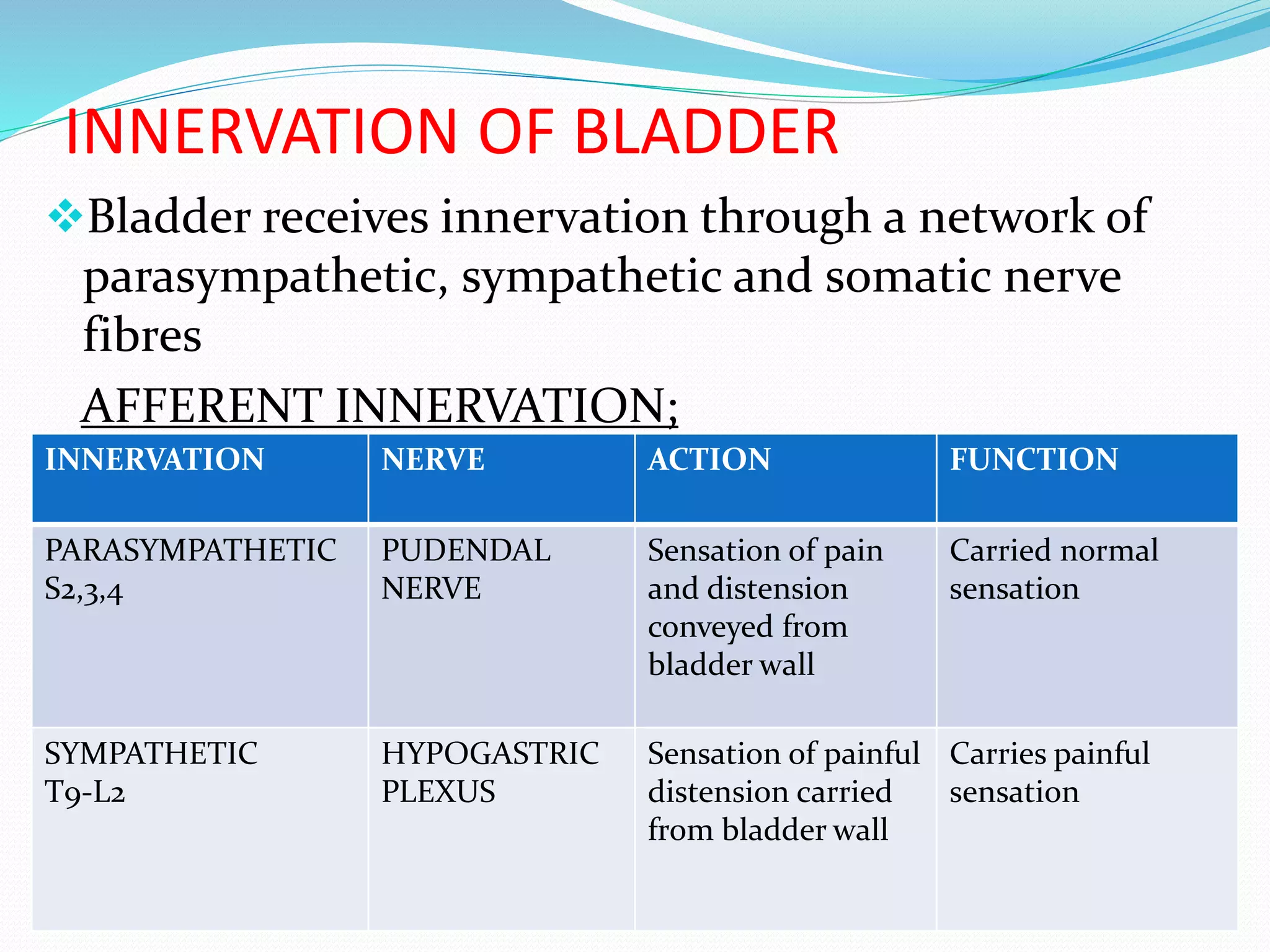
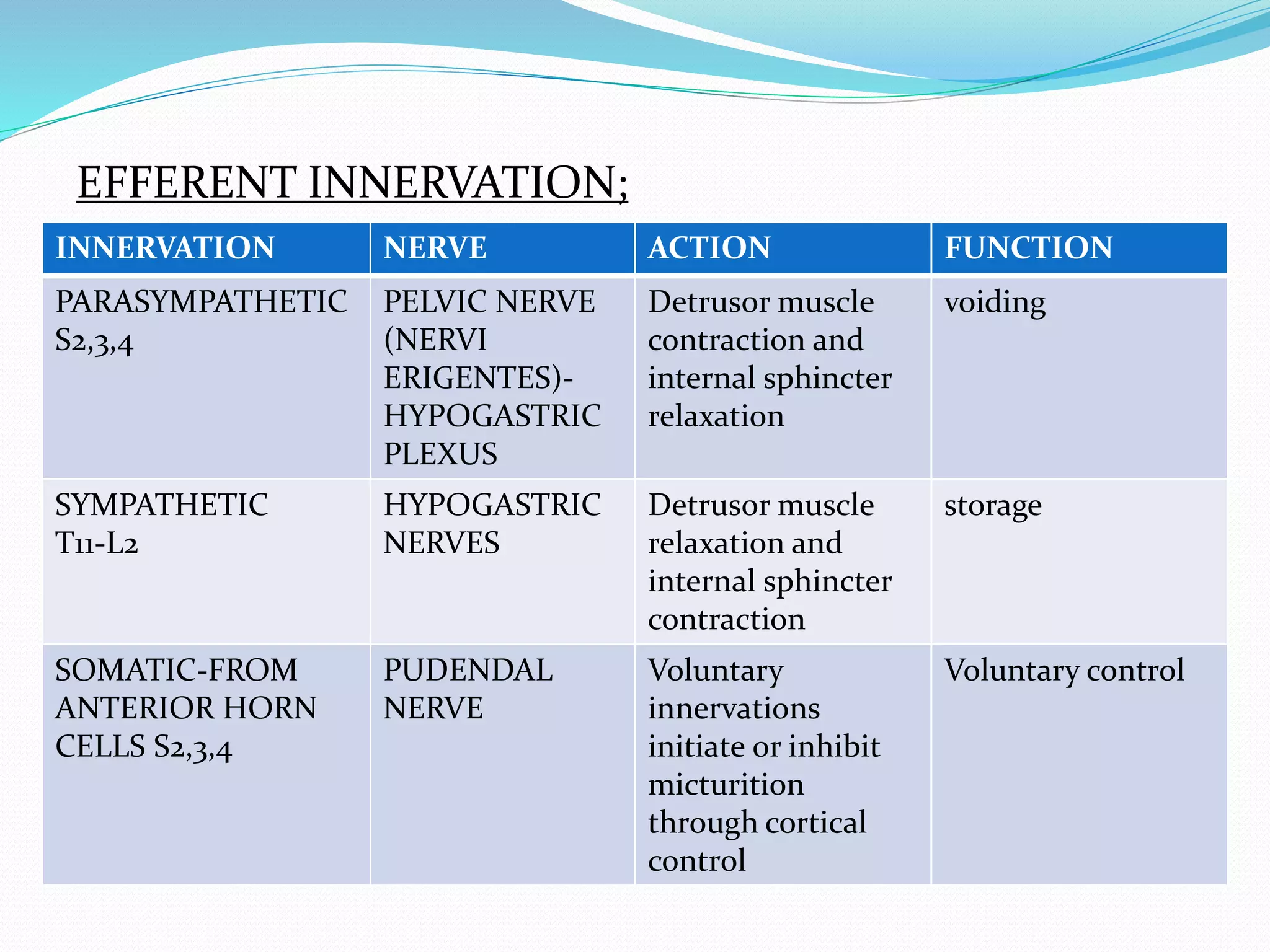
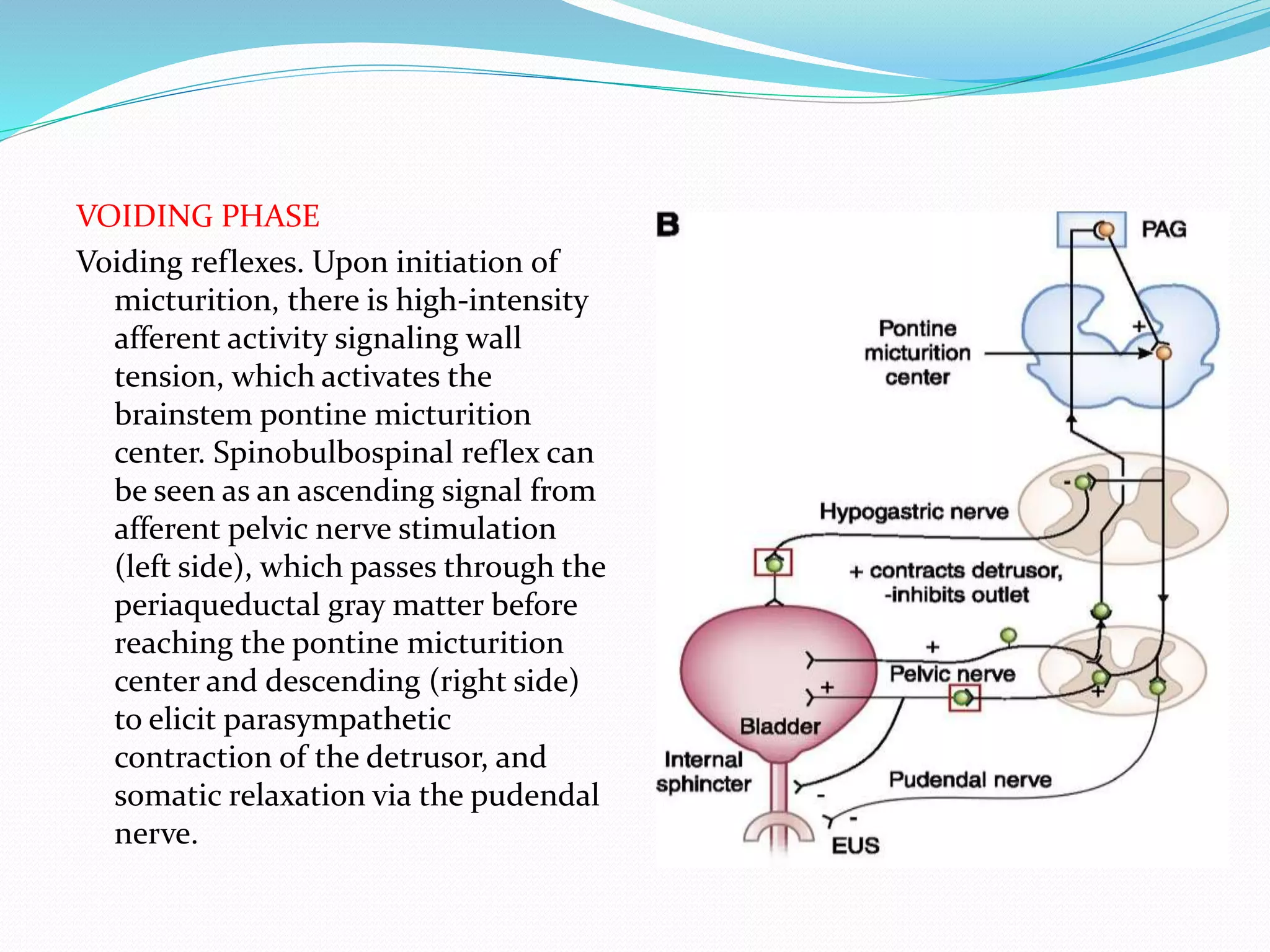
The document summarizes the anatomy and physiology of the bladder. It discusses the location and innervation of the bladder. It describes the storage and voiding phases of micturition and the roles of the sympathetic, parasympathetic and somatic nervous systems. It also discusses neurogenic bladder disorders and their classifications. Evaluation, complications and management of neurogenic bladder are outlined.