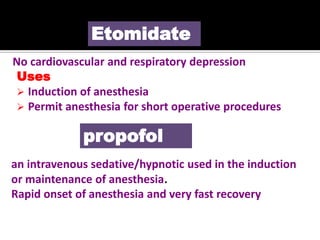
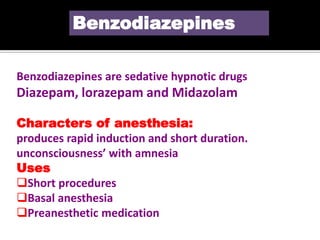
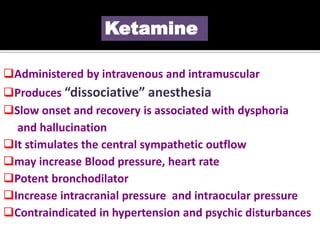
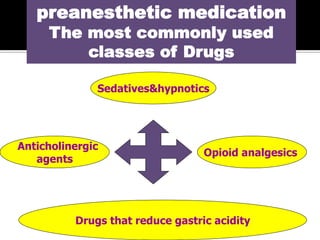
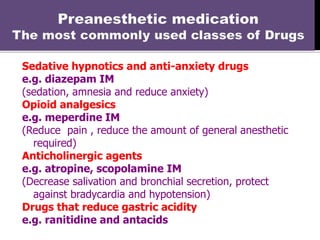
General anesthesia requires a combination of drugs to safely induce analgesia, amnesia, unconsciousness and muscle relaxation in patients. A balanced anesthesia approach uses multiple drugs together to benefit from their individual effects while minimizing adverse effects. Preanesthetic medication is commonly used before anesthesia to decrease anxiety, provide amnesia, relieve pain if present, and reduce risks associated with some anesthetic agents. It typically involves sedatives/hypnotics, opioid analgesics, anticholinergic agents, and drugs that reduce gastric acidity.