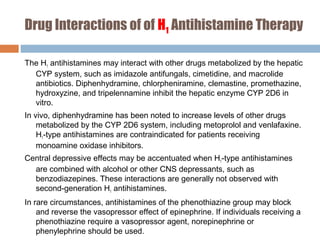
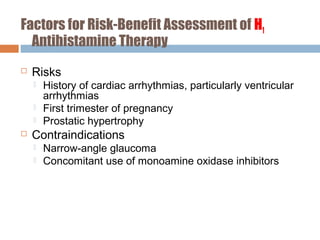
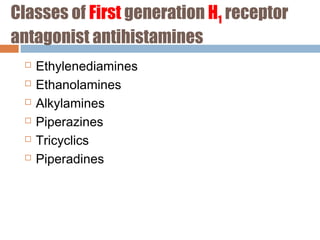
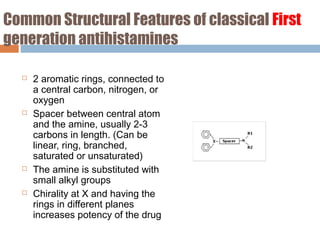
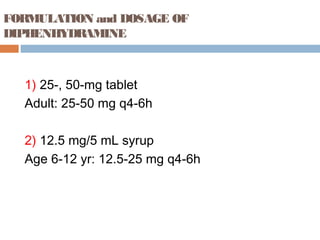
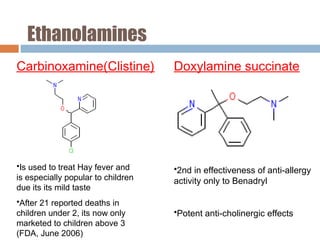
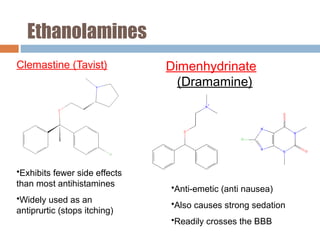
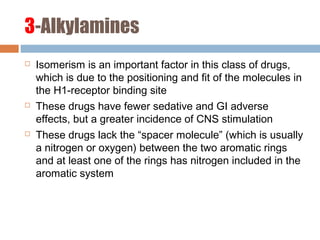
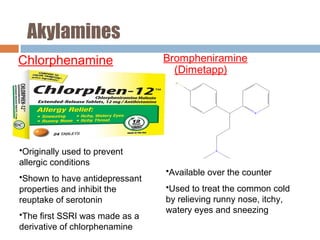
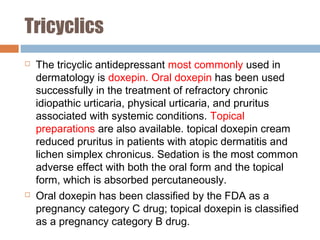
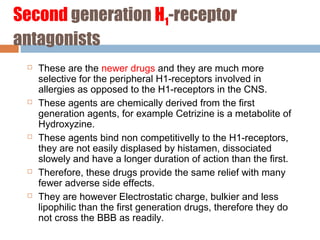
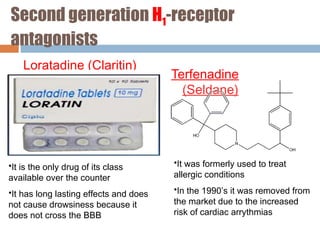
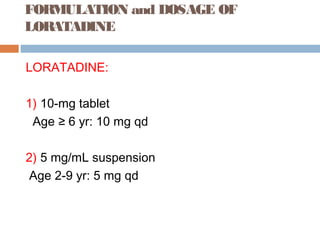
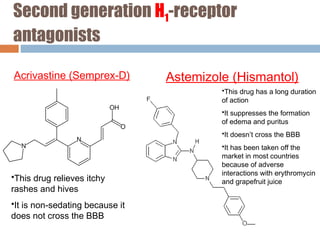
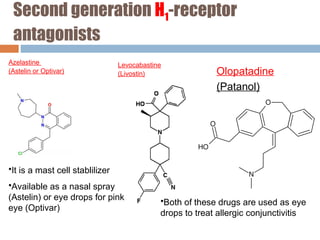
The document provides a comprehensive overview of antihistamines, detailing their definition, mechanisms of action, and various classes. It discusses the clinical uses, side effects, and contraindications of antihistamines, emphasizing the differences between first-generation and second-generation antihistamines. Special populations, drug interactions, and key examples of specific antihistamines are also covered.

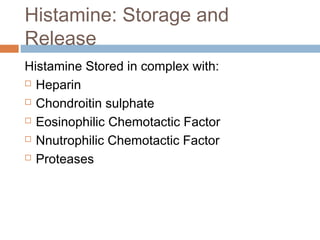
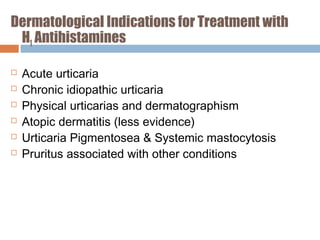
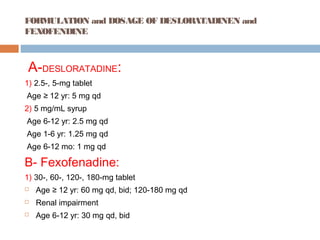
![H2-receptor antagonists
1-Cimetidine [Tagamet]
2-Ranitdine [Zantac]
3-Famotidine [Pepcid]
4-Nizatidine [Axid]](https://image.slidesharecdn.com/antihistaminepresentation-dr-180730184204/85/Antihistamine-presentation-45-320.jpg)