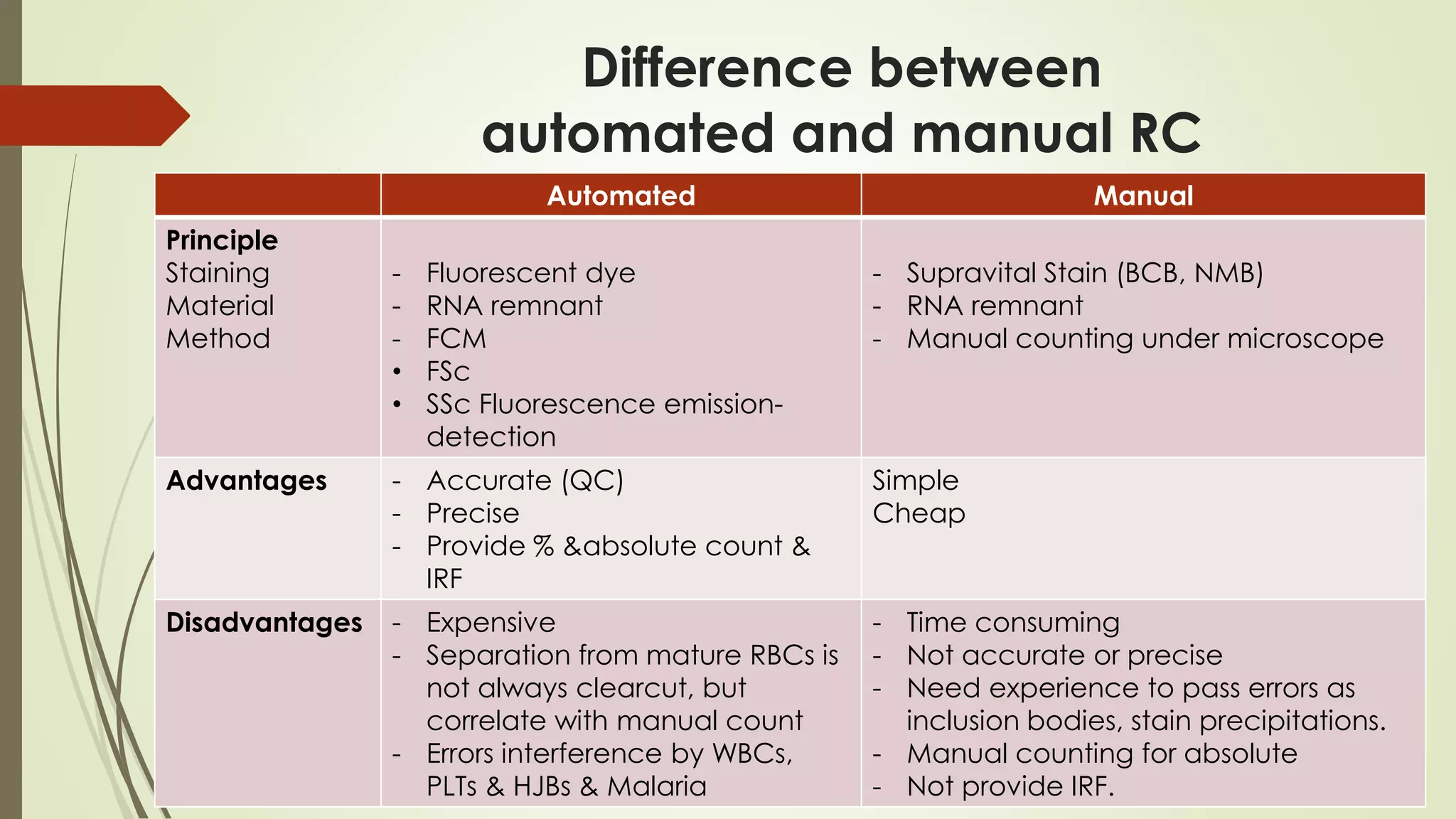
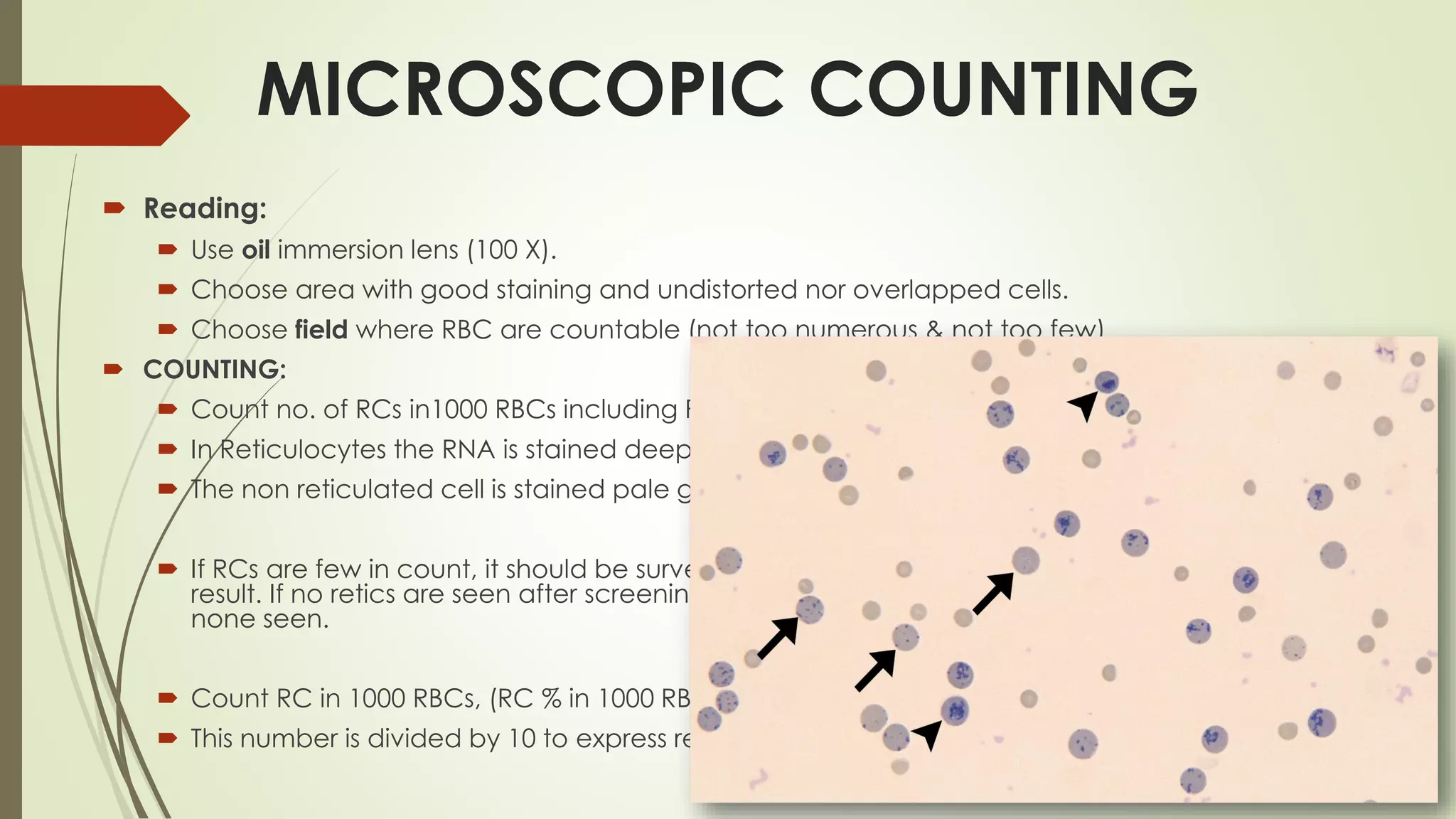
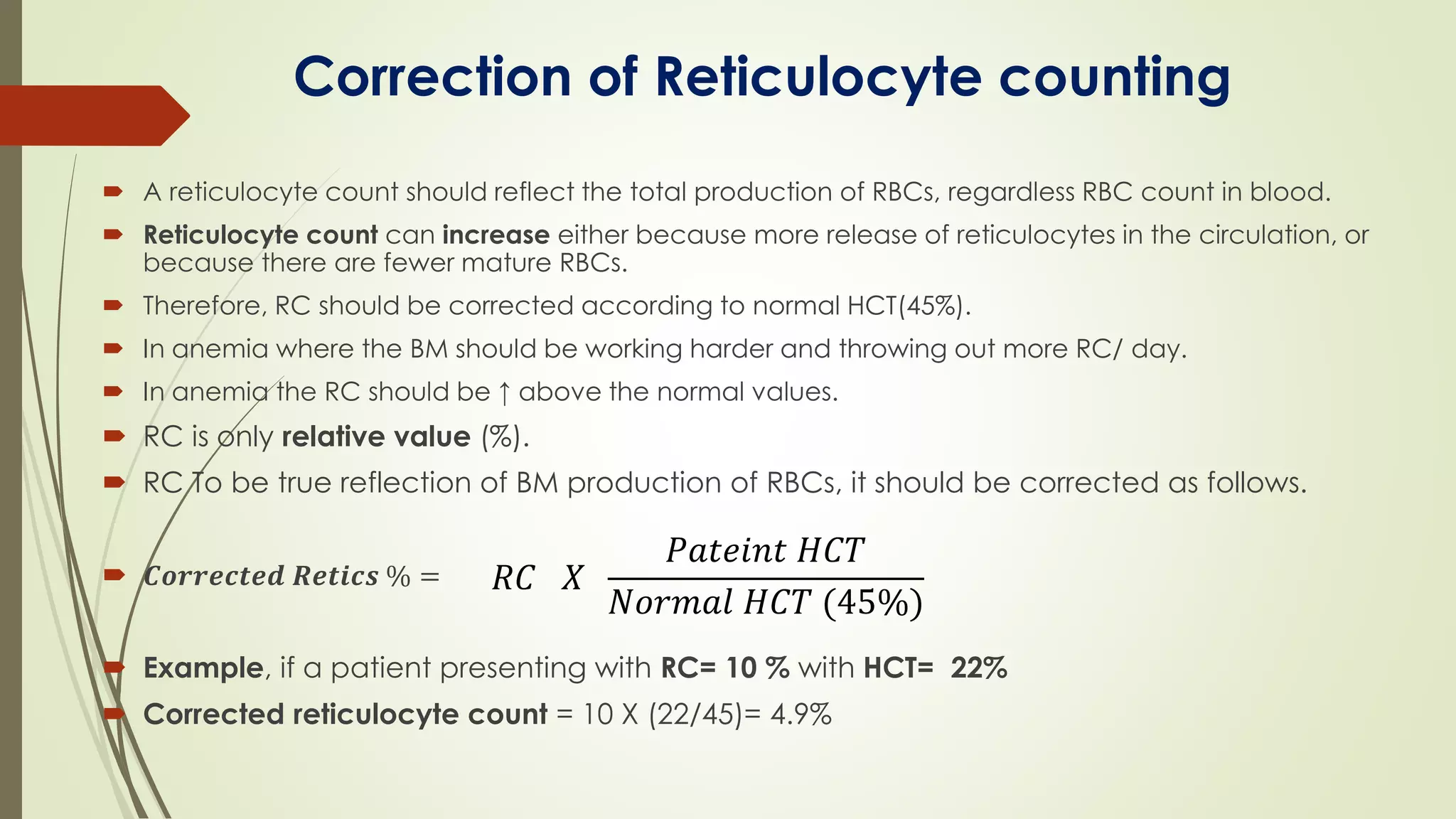
The document provides a comprehensive overview of reticulocytes, including their definition, maturation process, morphology, and counting methods both manual and automated. It emphasizes the significance of reticulocyte counts in assessing bone marrow activity and diagnosing anemia, detailing calculation methods such as corrected reticulocyte count and reticulocyte production index. Additionally, it discusses the different staining techniques, their implications, and the advantages and disadvantages of automated versus manual counting methods.
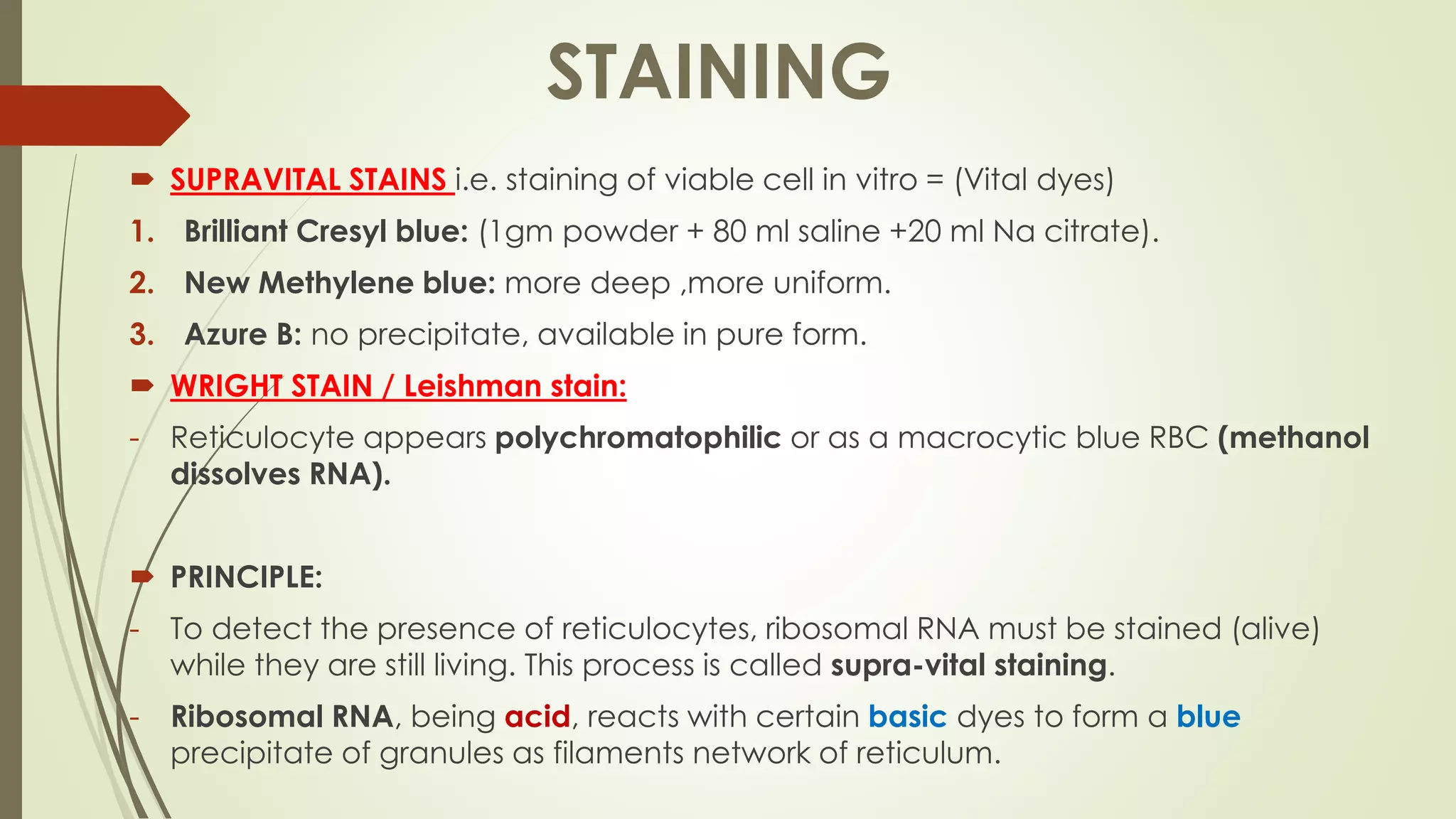
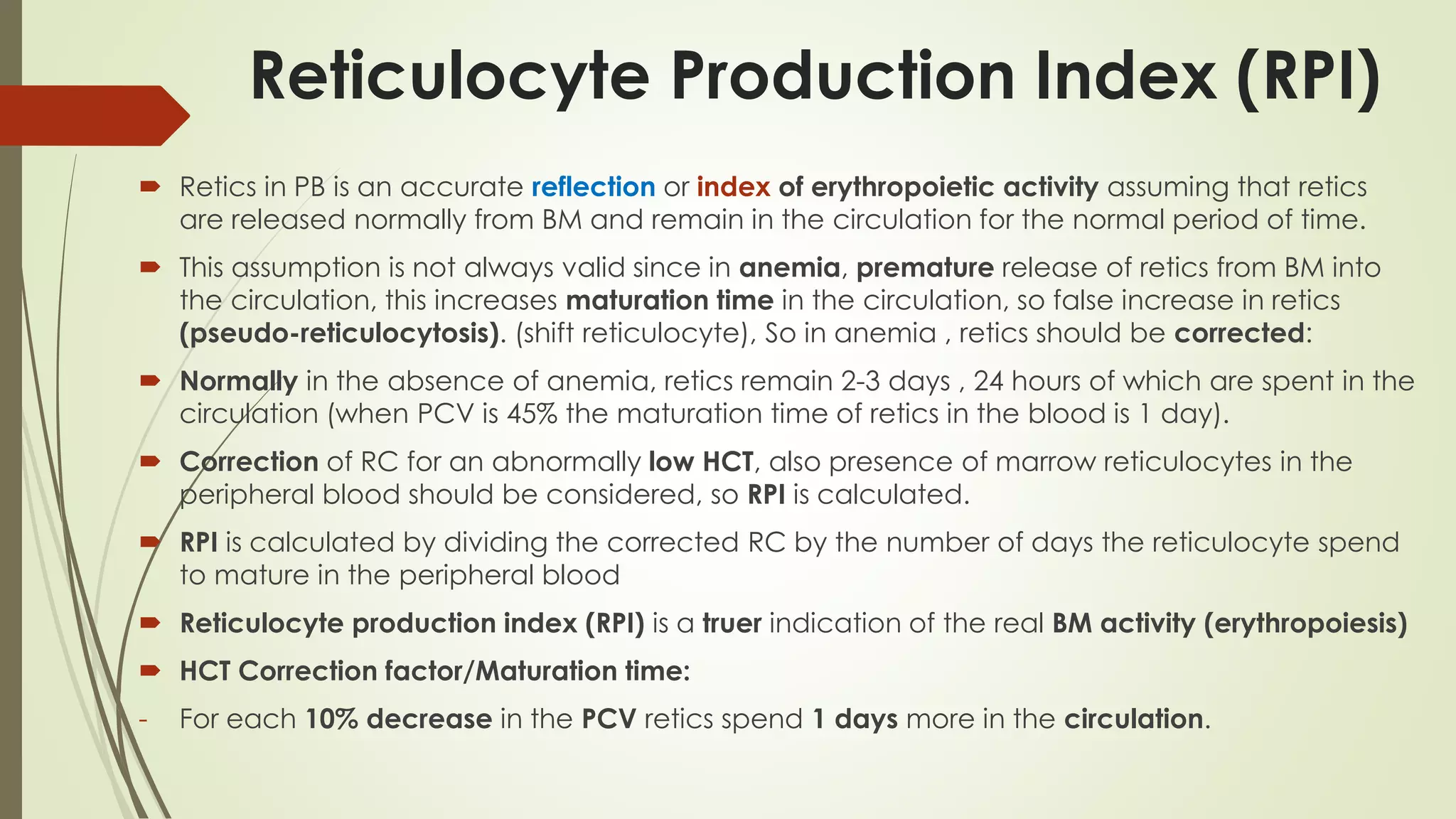
![ RPI =
RPI =
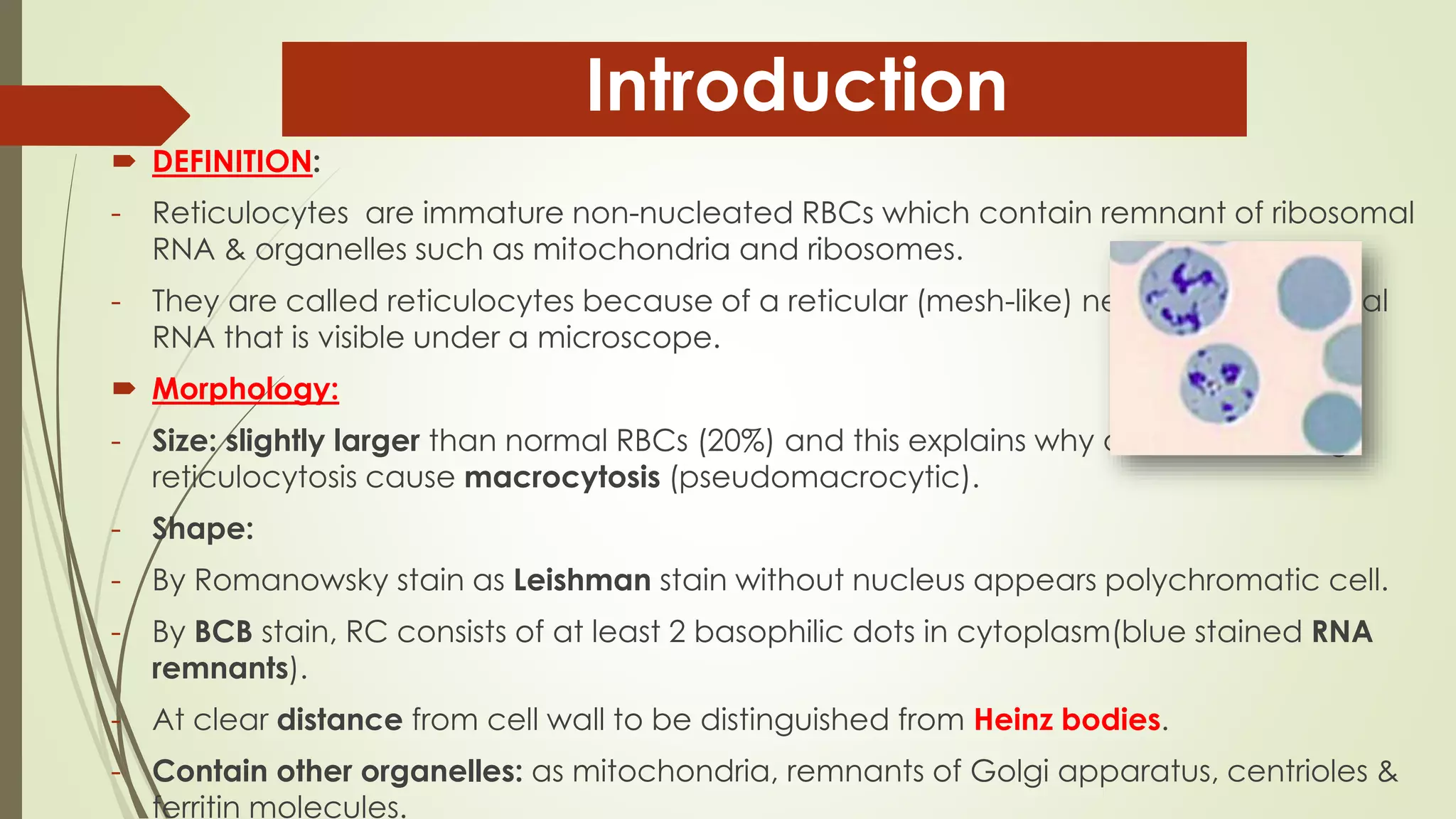
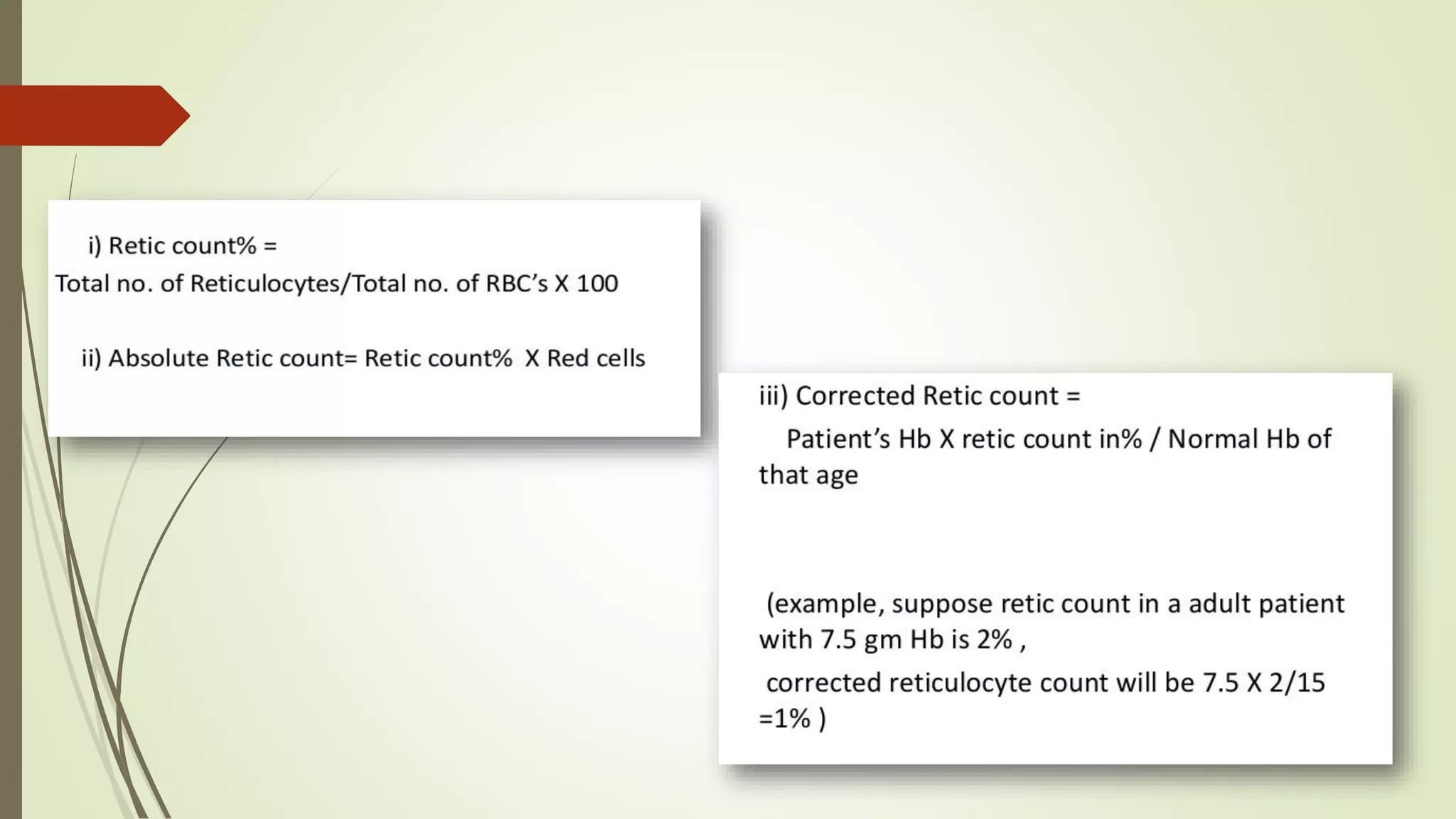
Retic Production Index (RPI) = Corrected retic count (%) / # Days (Maturation time)
For example, a patient with a RC 10% and a HCT 25% would yield an
RPI of :
RPI = 10% X ( 25%/ 45%) / 2 = 2.7
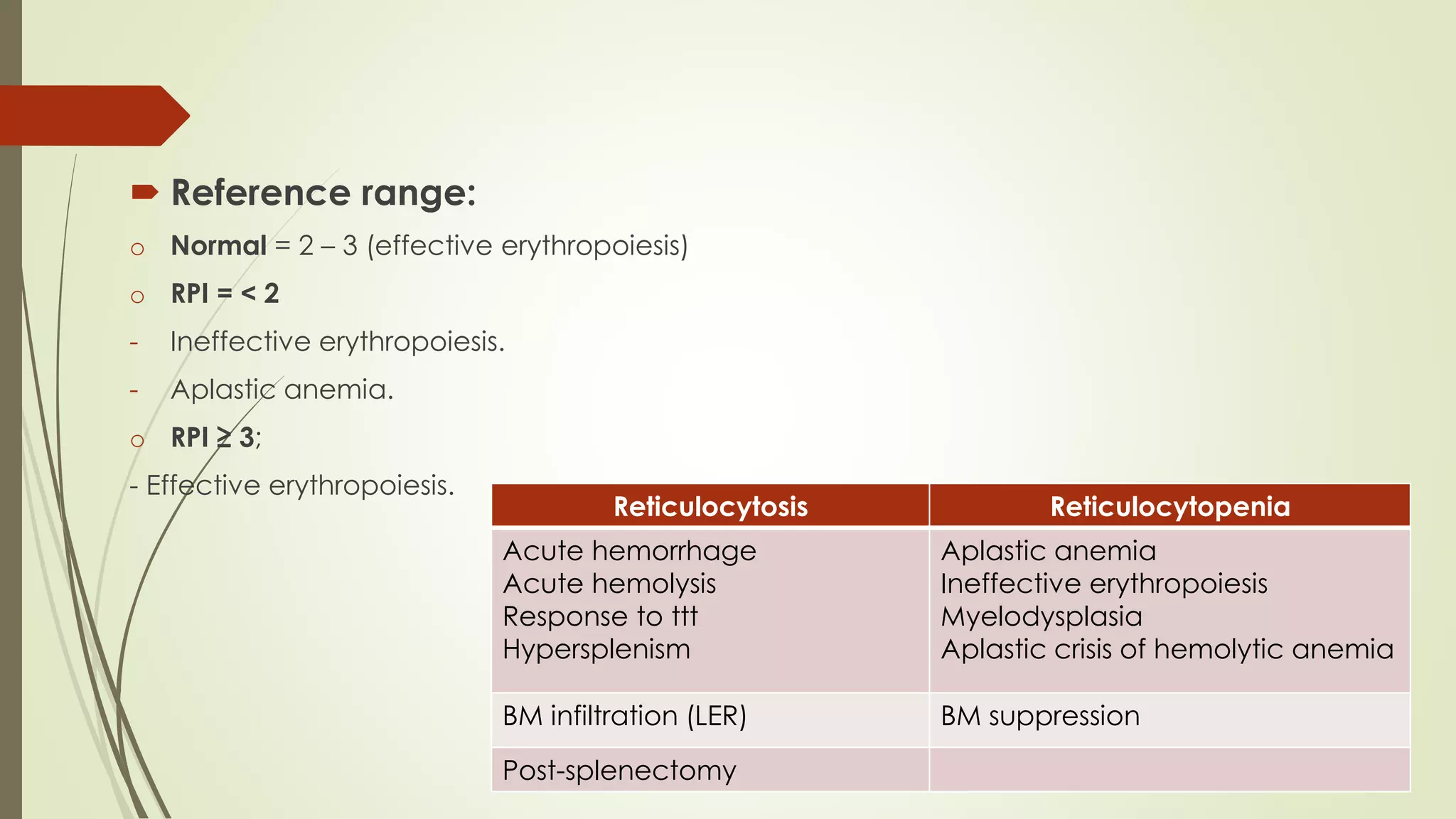
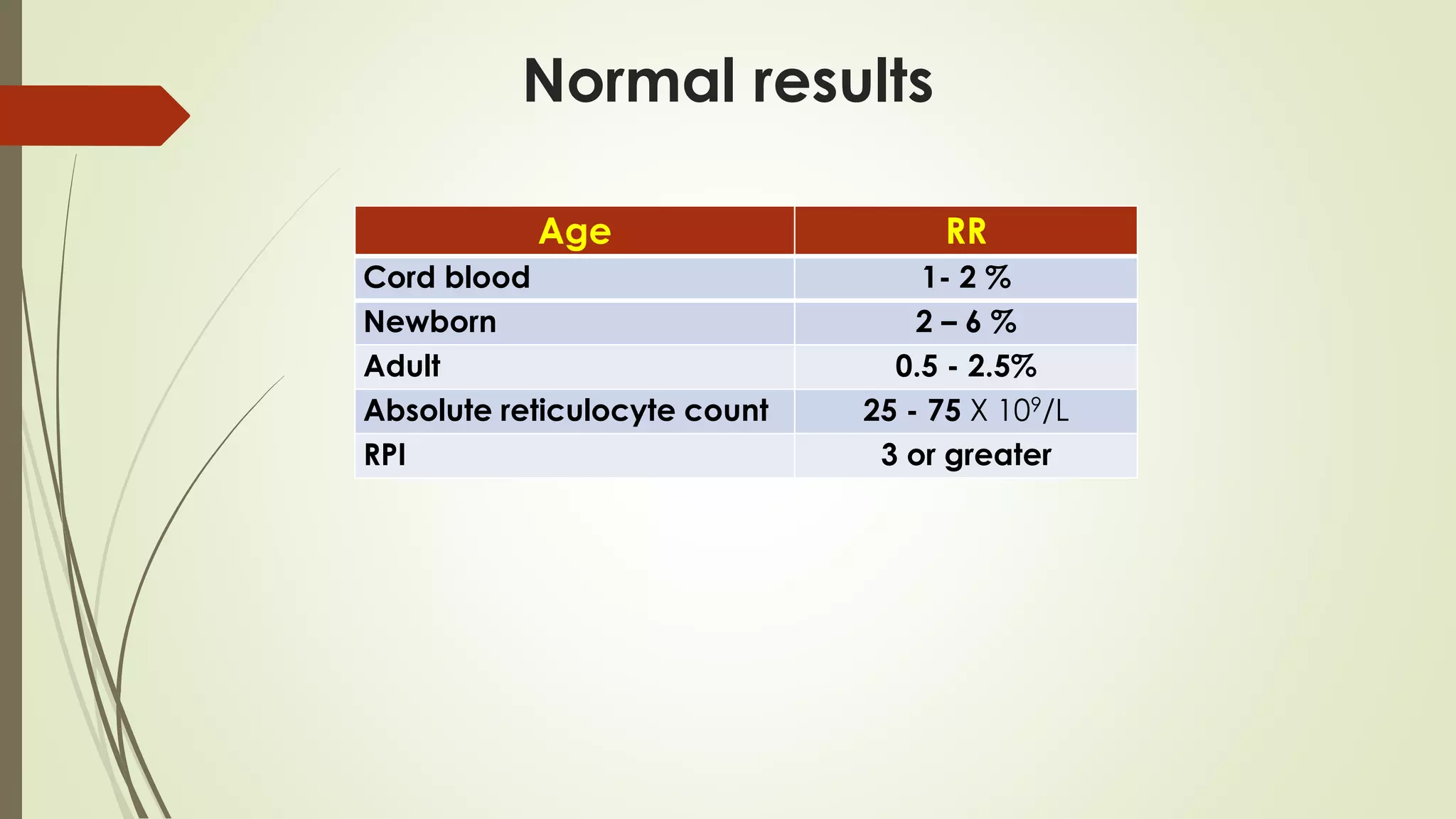
Reticulocyte Production index (RPI)
HCT Maturation time
or
HCT Correction factor
PCV 45-36% 1 day
PCV 35-26% 1.5 days
PCV 25-16% 2 days
PCV ≤15% 2.5 days
[𝑅𝐶 𝑋
𝑃𝑎𝑡𝑒𝑖𝑛𝑡 𝐻𝐶𝑇
𝑆𝑡𝑎𝑛𝑑𝑎𝑟𝑑 𝐻𝐶𝑇
] / Maturation index (correction factor)
𝐶𝑜𝑟𝑟𝑒𝑐𝑡𝑒𝑑 𝑅𝐶
𝑀𝑎𝑡𝑢𝑟𝑎𝑡𝑖𝑜𝑛 𝑡𝑖𝑚𝑒](https://image.slidesharecdn.com/4-reticulocyticcount-230404230920-c9af706c/75/Reticulocytic-count-pdf-18-2048.jpg)