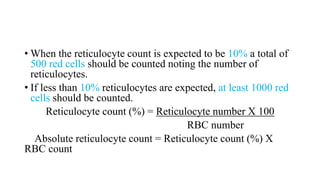
Reticulocyte count is a measure of red blood cell production in the bone marrow. Reticulocytes are immature red blood cells that contain remnants of ribosomal RNA. The reticulocyte count is performed by staining a blood sample with new methylene blue dye, which causes the RNA in reticulocytes to appear blue under a microscope. The number of reticulocytes is then counted and calculated as a percentage of total red blood cells. An increased reticulocyte count (reticulocytosis) indicates the bone marrow is actively producing new red blood cells in response to blood loss or destruction. A decreased reticulocyte count suggests the bone marrow