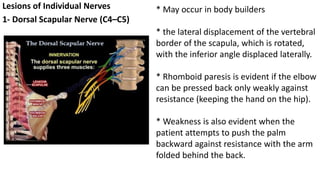
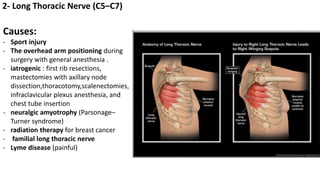
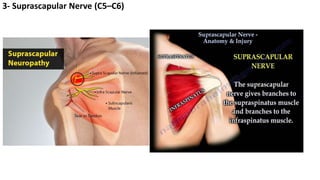
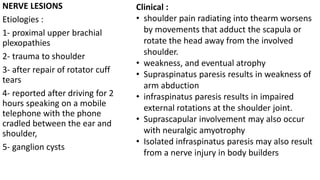
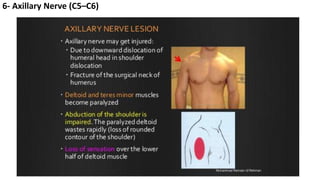
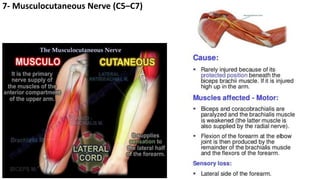
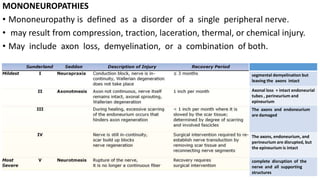
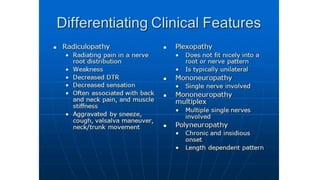
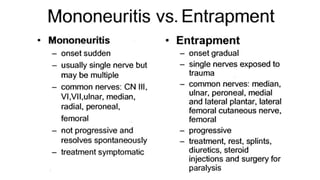
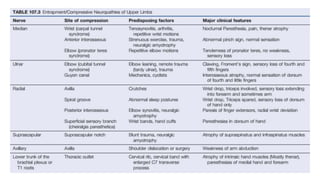
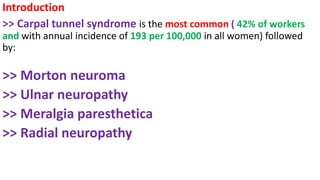
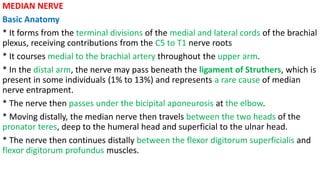
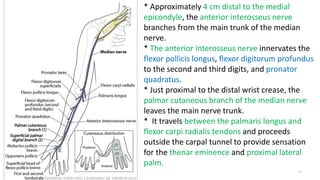
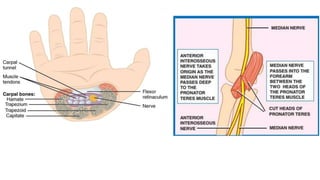
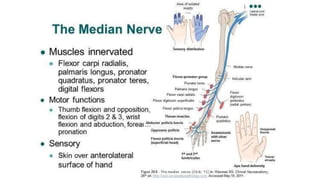
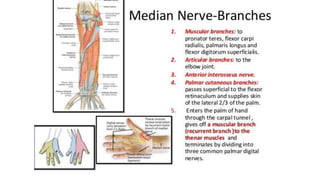
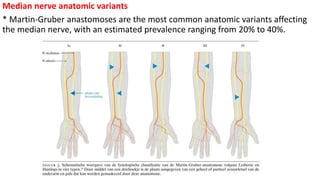
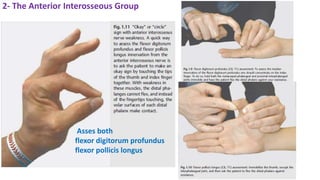
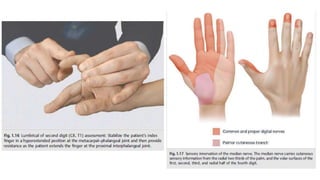
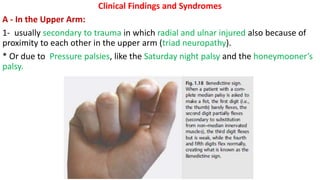
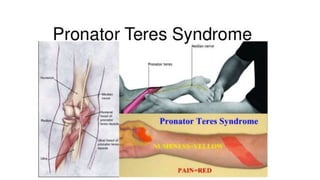
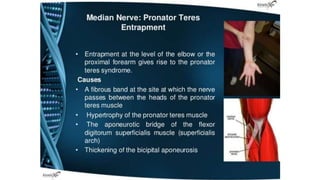
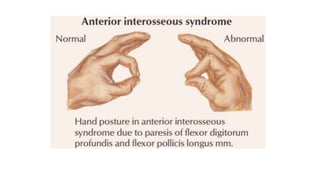
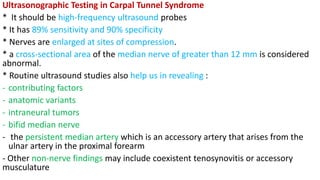
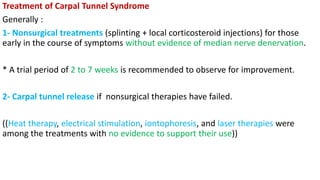
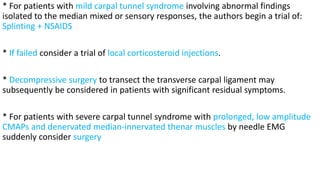
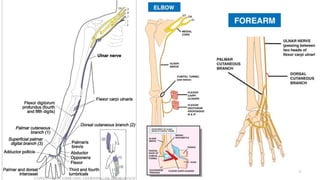
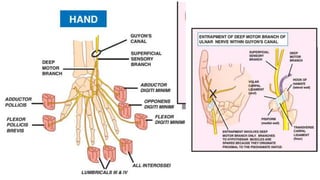
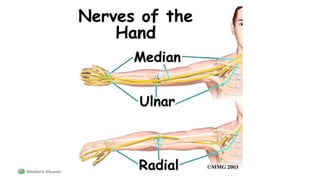
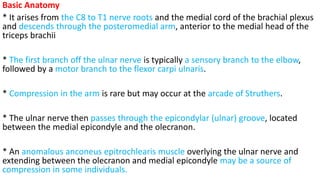
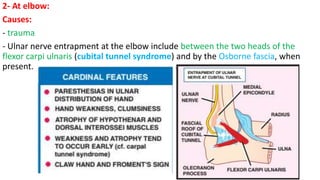
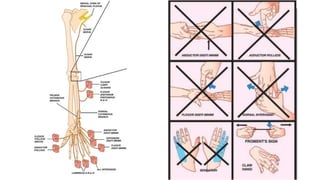
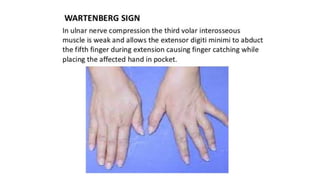
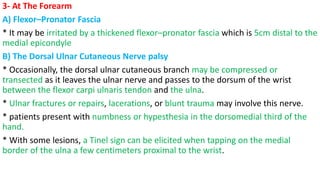
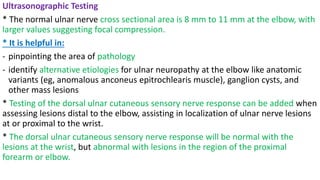
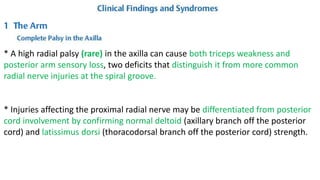
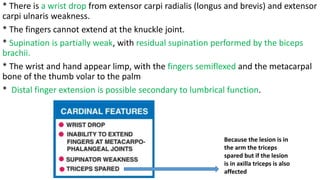
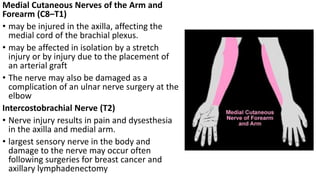
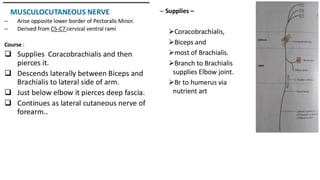
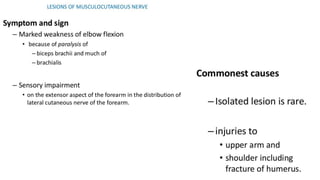
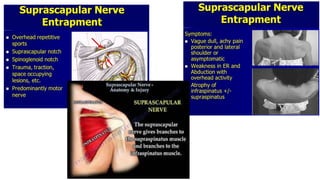
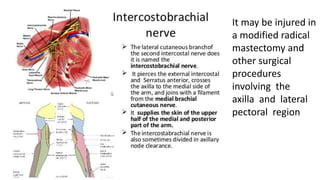
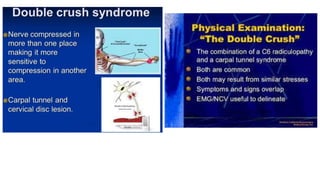
This document discusses peripheral nerve diseases, focusing on individual nerve lesions. It describes the anatomy and clinical presentations of lesions of the dorsal scapular, long thoracic, suprascapular, subscapular, thoracodorsal, anterior thoracic, axillary, musculocutaneous, and median nerves. It also discusses median nerve variants, carpal tunnel syndrome, and ulnar nerve anatomy.