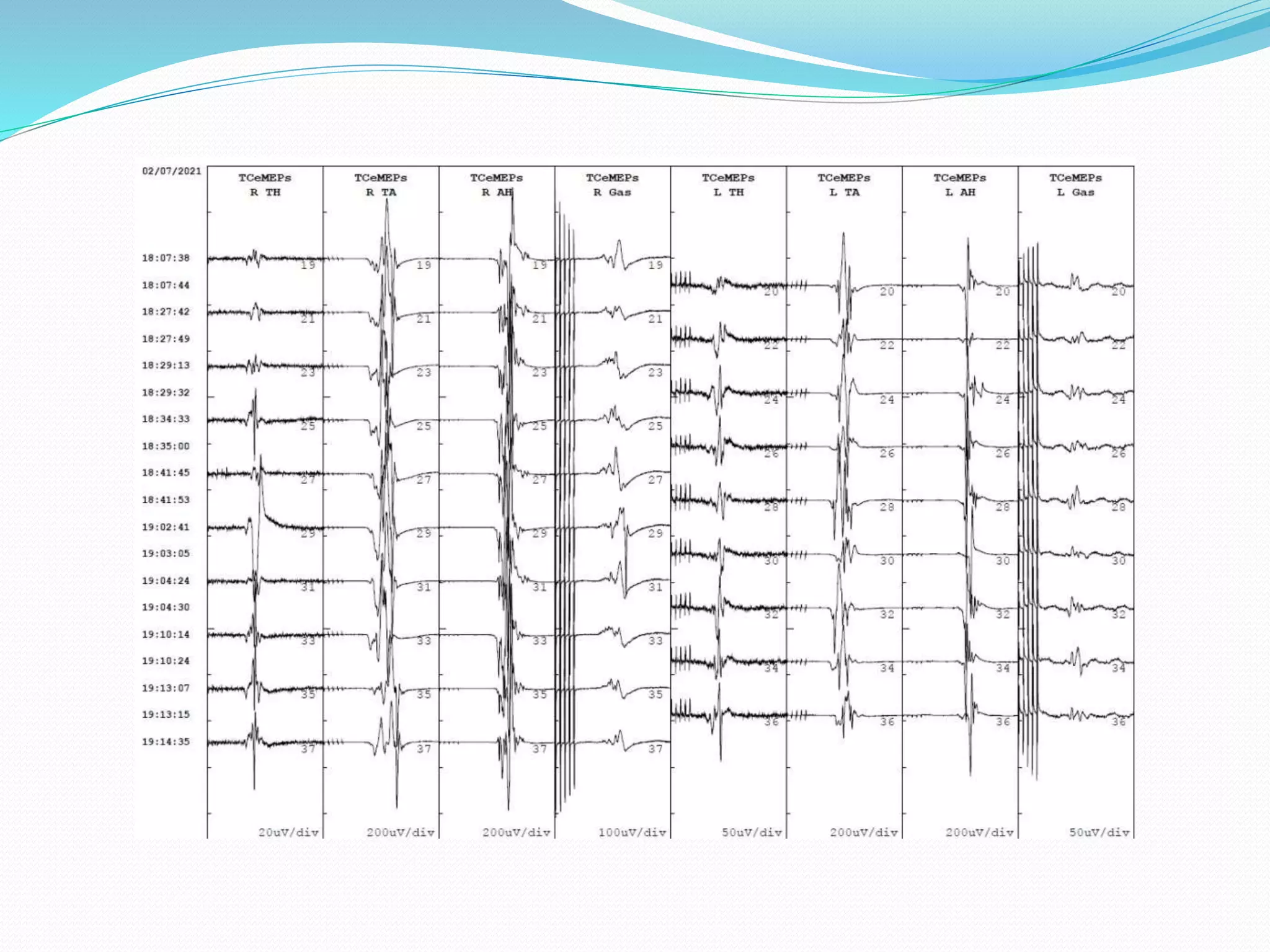
This document discusses intraoperative neurophysiological monitoring during three spinal surgeries. In the first case, neurotonic discharges and a drop in motor evoked potentials alerted surgeons to a problem with a screw placement, catching a mild postoperative deficit. In the second case, signals recovered after repositioning a retractor. In the third case, changes in motor evoked potentials led surgeons to abort the procedure, likely preventing neurological injury. The conclusion emphasizes that multimodal monitoring including SSEPs, EMG, and MEPs provides good detection of issues compared to any single method.