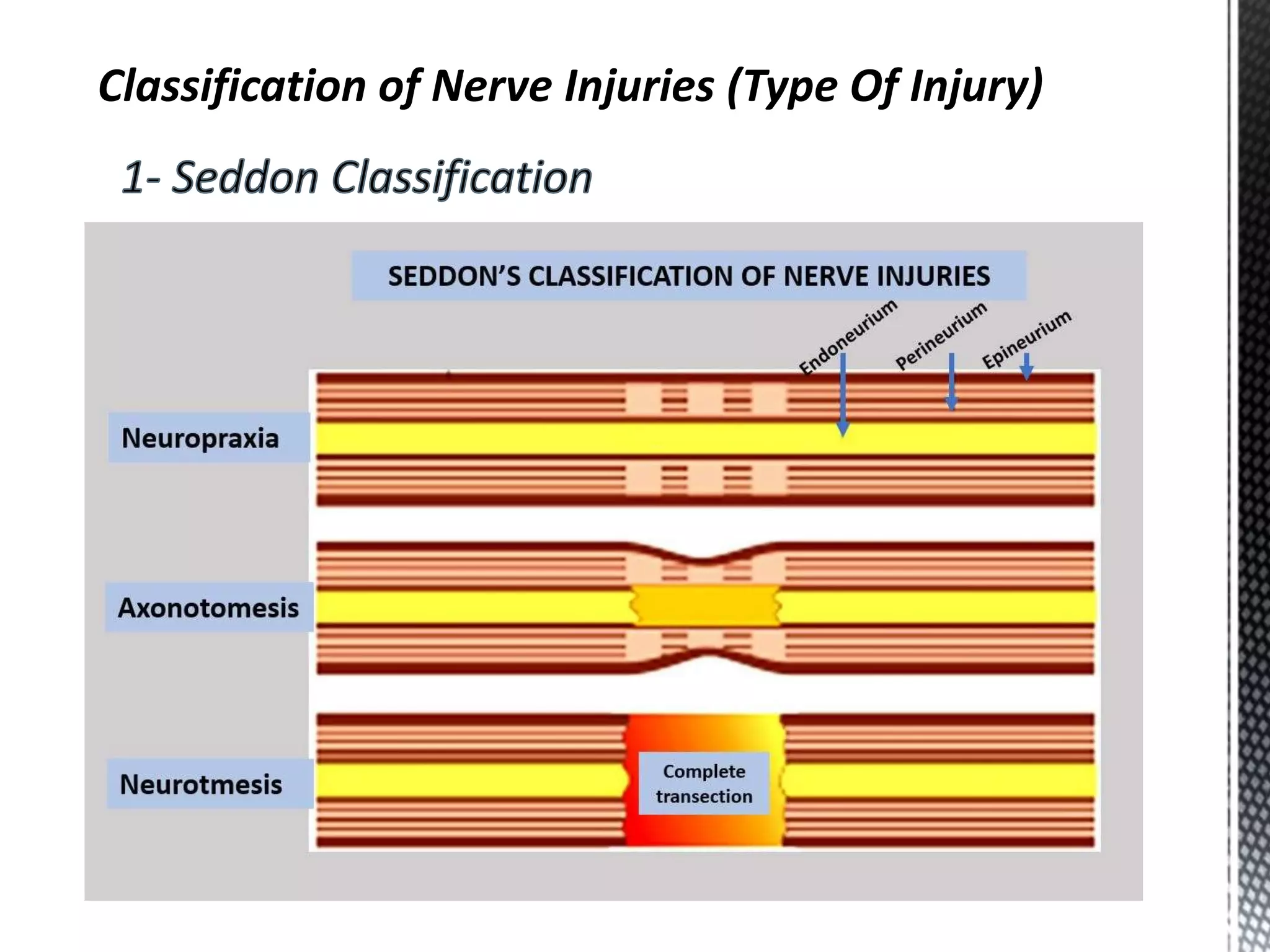
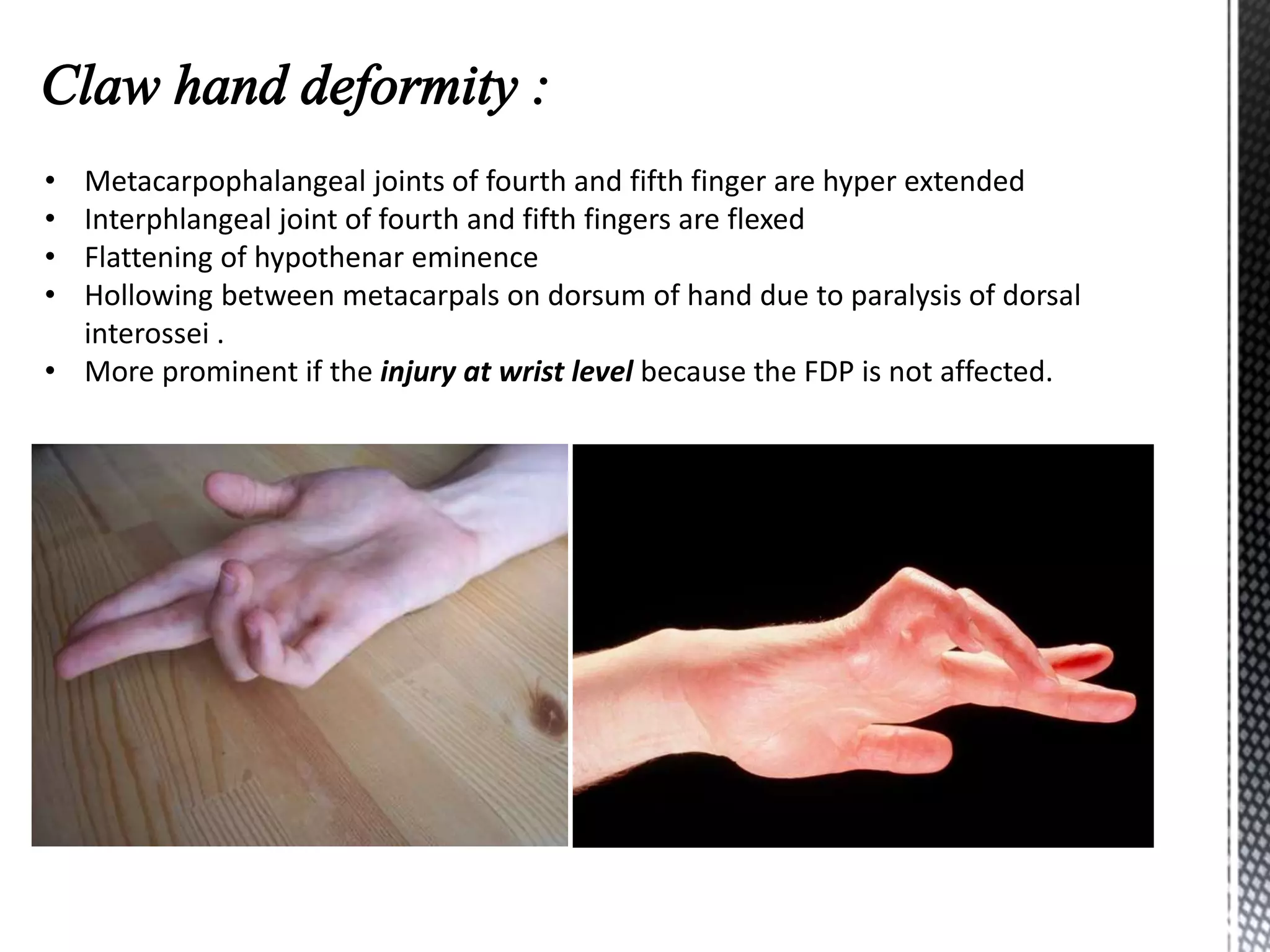
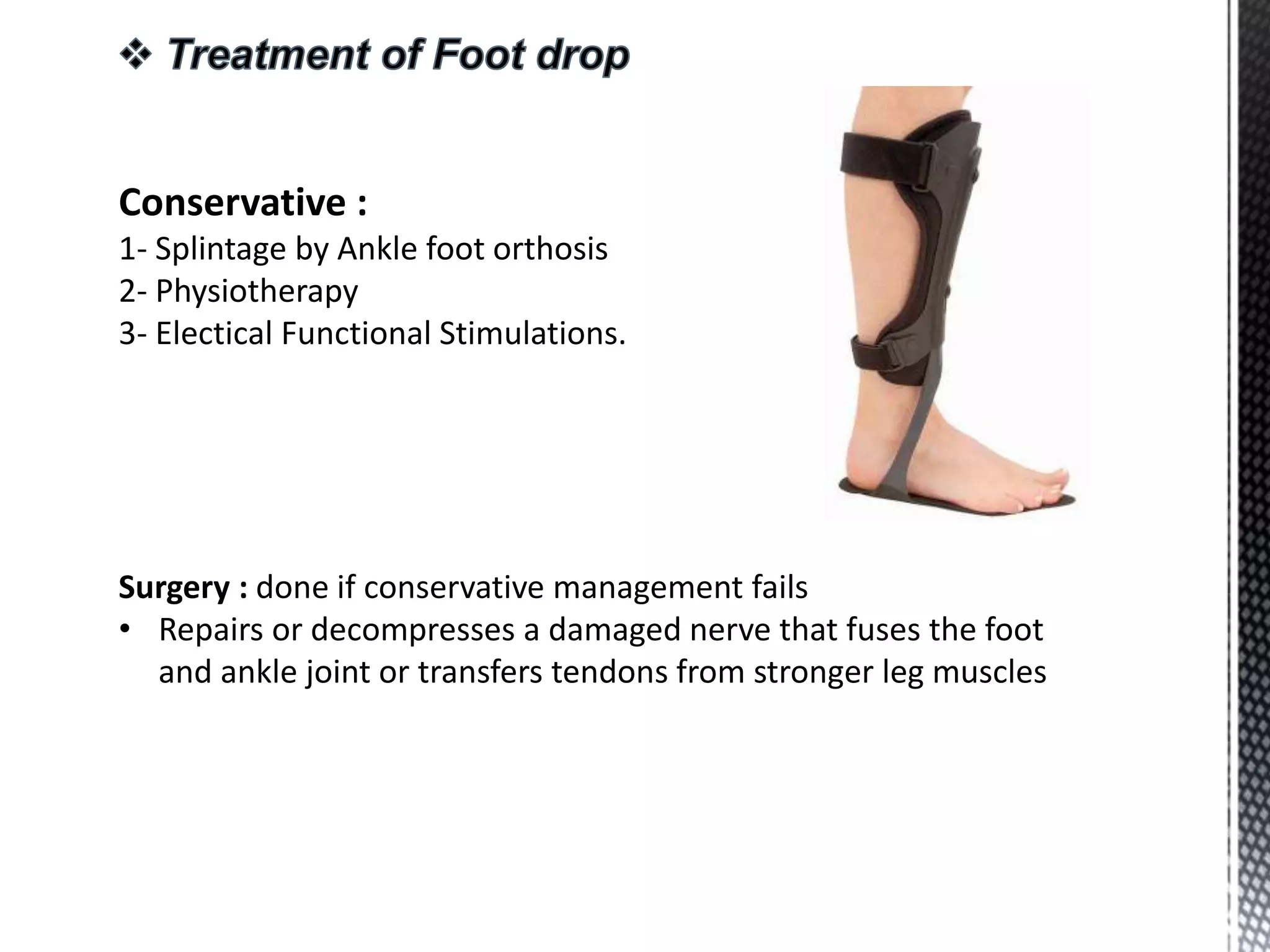
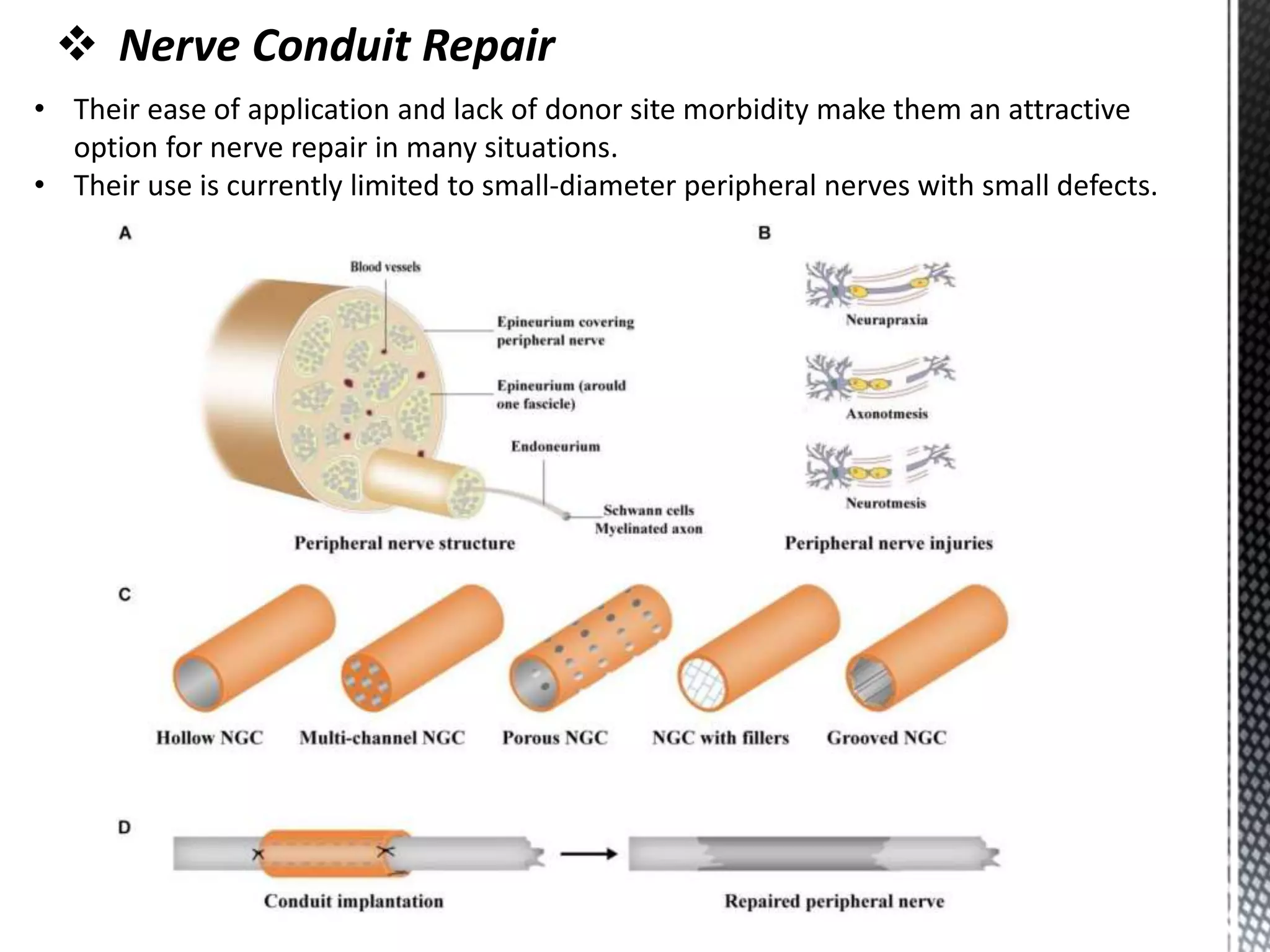
This document provides information on the diagnosis and classification of nerve injuries, as well as details on specific nerves including their anatomy, causes of injury, clinical features, and management approaches. It discusses the axillary, radial, ulnar, median, sciatic, femoral, and lumbosacral plexus nerves. Diagnosis involves history, examination, and investigations such as nerve conduction studies, electromyography, and imaging. Surgical management of nerve injuries includes neurolysis, nerve repair, grafting, and the use of nerve conduits.