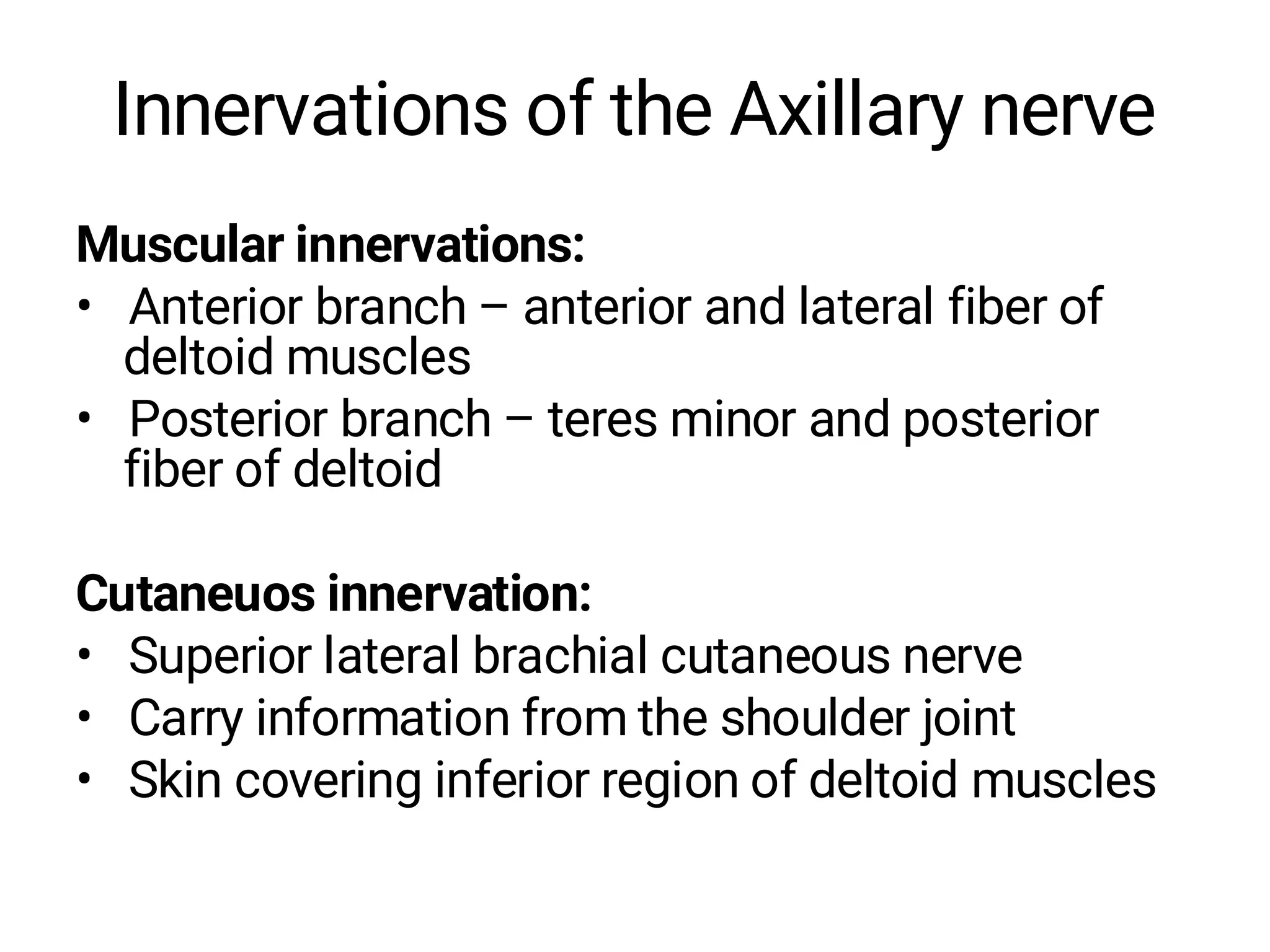
The document discusses the major nerves of the upper limb that originate from the brachial plexus, including the axillary nerve, musculocutaneous nerve, radial nerve, median nerve, and ulnar nerve. It describes the motor and sensory innervation for each nerve, as well as common injuries and clinical presentations associated with damage to each nerve, such as median nerve palsy resulting in "ape hand" deformity or ulnar nerve palsy causing clawing of the ring and little fingers. The document provides an overview of the anatomy and function of the main nerves of the upper extremity.