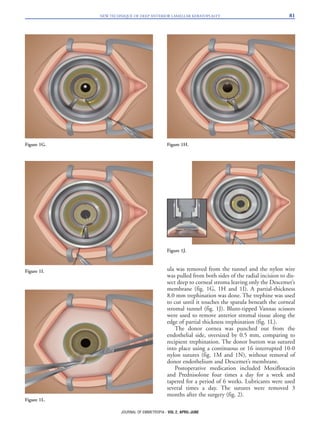
The document presents a new technique for deep anterior lamellar keratoplasty (DALK) aimed at improving corneal replacement by preserving the host's endothelial layer, especially beneficial for keratoconus patients. It describes a surgical procedure using a combination of a diamond knife and a nylon wire to create a smooth separation of the corneal stroma from Descemet's membrane, overcoming limitations of early DALK methods. This innovative technique offers a shorter learning curve for surgeons and aims to ensure better visual outcomes with fewer complications compared to traditional methods.