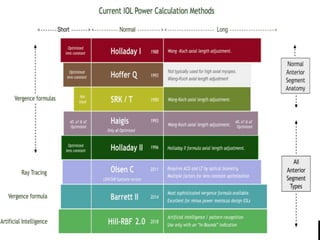
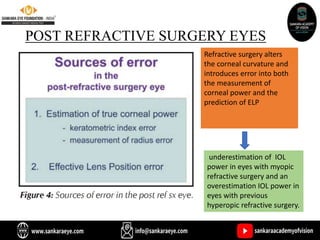
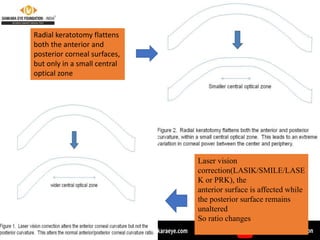
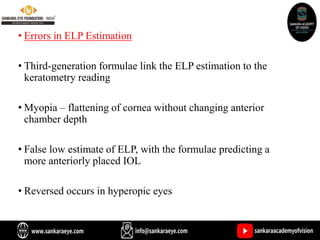
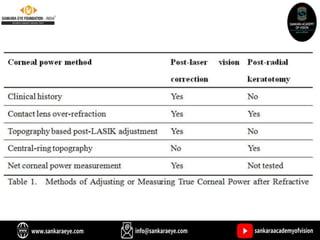
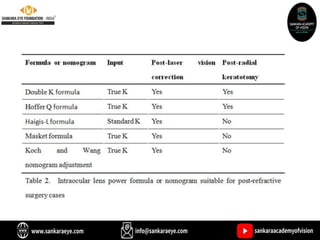
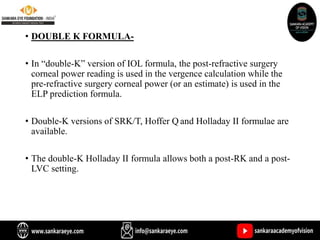
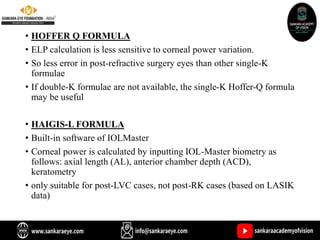
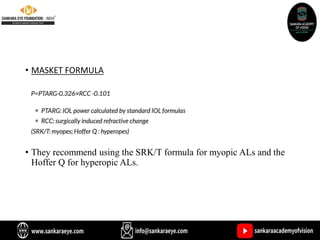
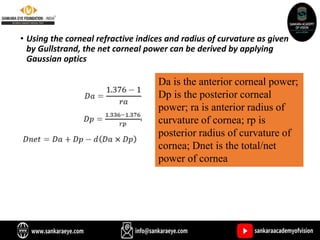
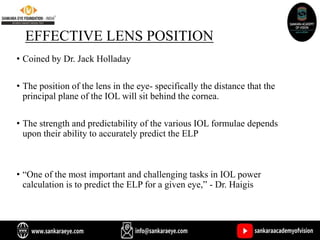
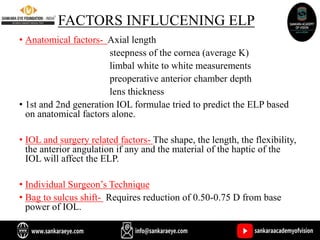
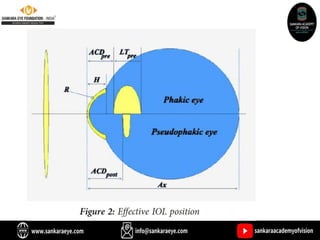
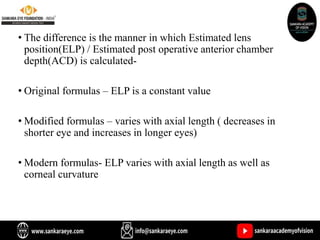
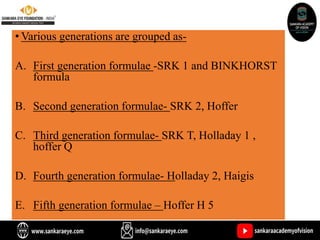
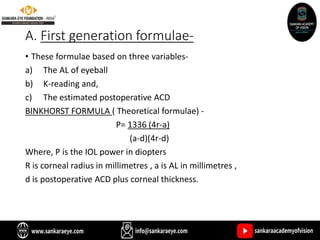
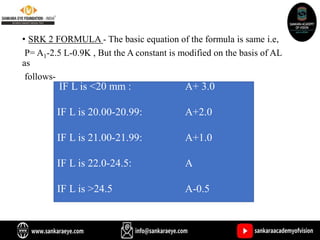
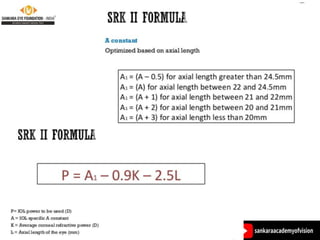
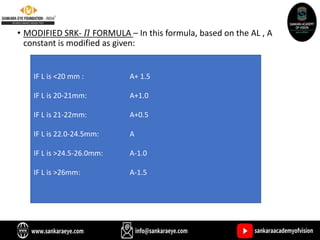
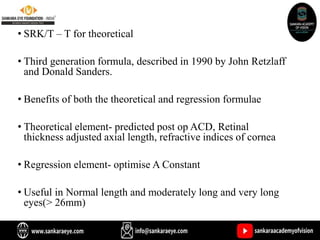
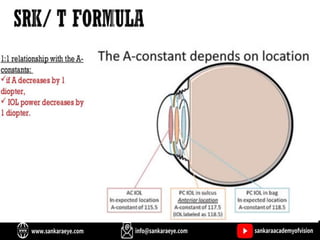
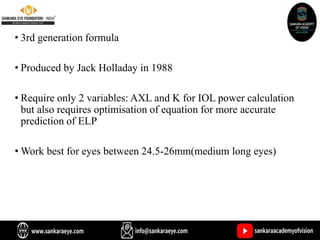
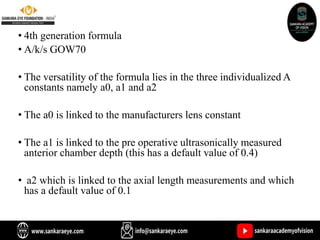
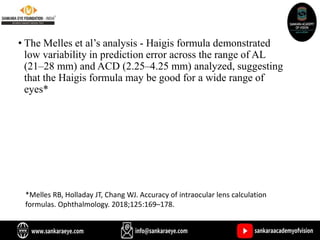
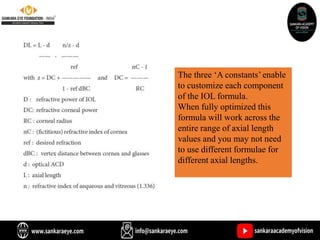
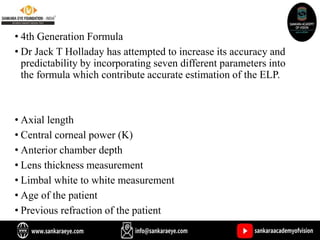
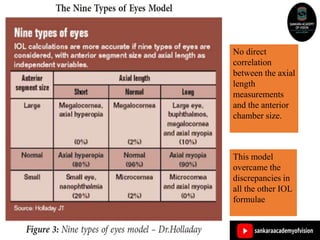
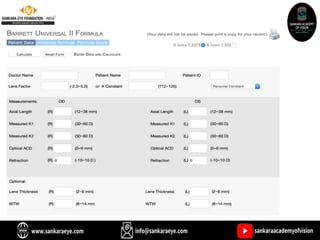
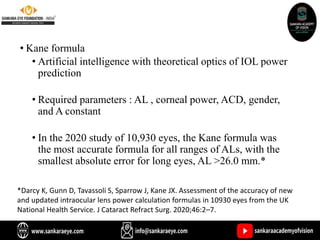
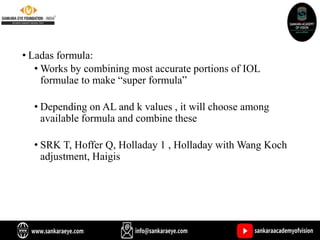
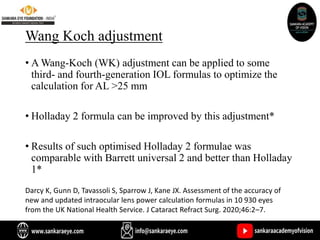
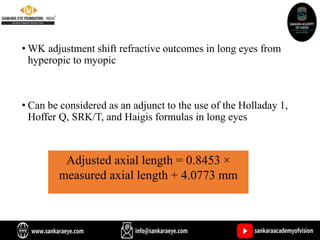
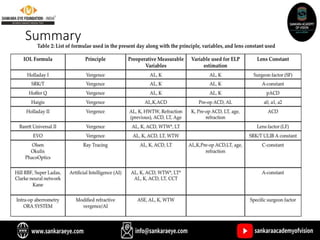
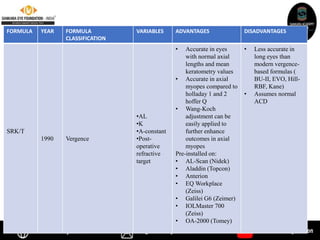
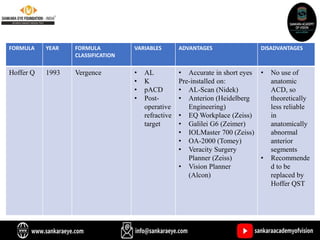
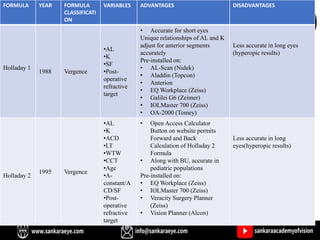
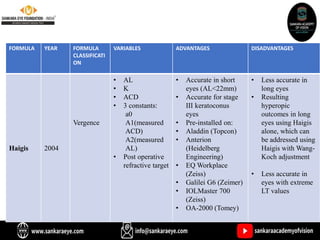
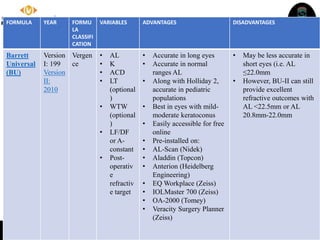
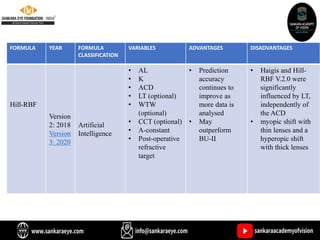
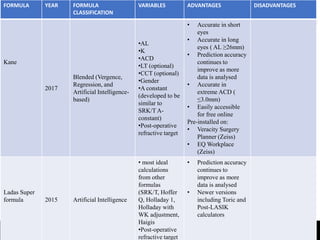
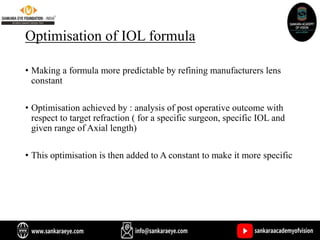
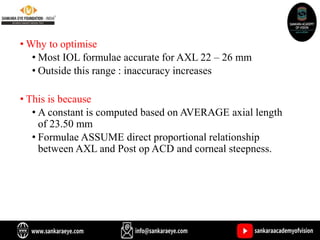
The document discusses various intraocular lens (IOL) calculation formulas used for cataract surgery, detailing their historical development and mathematical foundations. It explores different generations of formulas, including theoretical, regression, and AI-driven methods, highlighting factors affecting effective lens position and the importance of accurate biometric measurements. Additionally, it explains the adaptation of IOL power based on anatomical and surgical factors, ensuring optimal refractive outcomes for patients.










![PIGGY-BACK IOLS
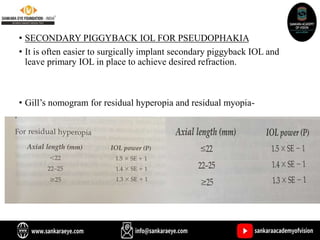
• Post IOL refractive surprise or in those with large dioptric
requirement, a piggy back IOL in sulcus can be placed along with the
primary implant.
• Myopic correction: P = 1.0 x Error
• Hyperopic correction: P = 1.5 x Error
Where P = the needed power in the piggyback lens Error = the residual
refractive error that needs to be corrected
Findl O , Menapace R. Piggyback intraocular lenses [letter].JCataract Refract SLlrg. 2000;26(3): 308~30 9.
Findl O , Menapace R, Rainer G, Georgopoulos M. Contact zone of piggyback acryliCintraocular lenses. , Cataract
Refract Surg. 1999;25(6):860- 862](https://image.slidesharecdn.com/biometry-iolpowerandcalculationfinalppt-230903135810-82f20ed5/85/Biometry-Iol-power-and-calculation-final-ppt-pptx-121-320.jpg)