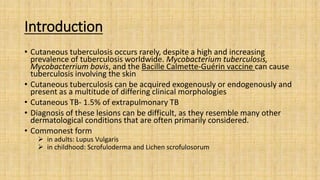
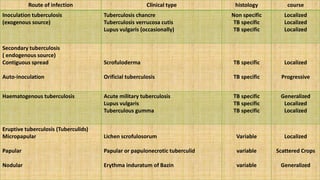
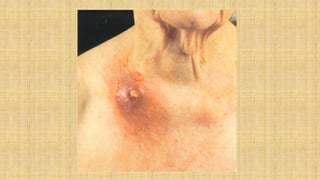
Cutaneous tuberculosis can present in various forms as a result of hematogenous spread or direct extension from a latent tuberculosis infection. Common types include lupus vulgaris, verrucosa cutis, and scrofuloderma. Diagnosis involves skin biopsy demonstrating tuberculoid granulomas with occasional acid-fast bacilli. Treatment consists of long-term multidrug antitubercular therapy following standard protocols for systemic tuberculosis.