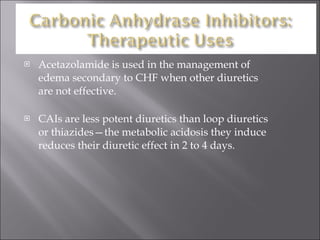
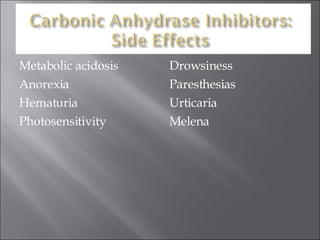
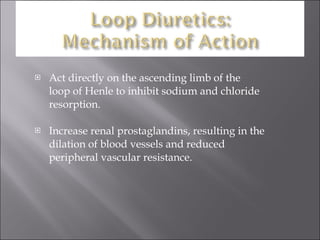
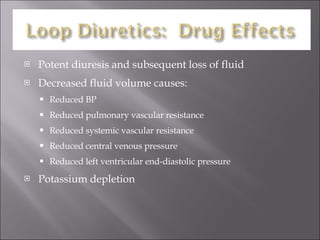
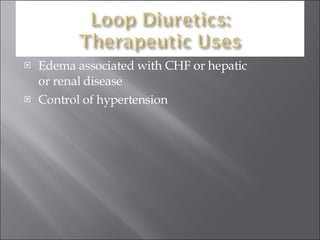
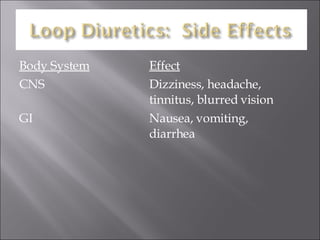
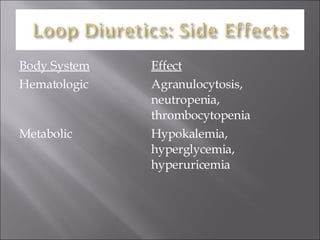
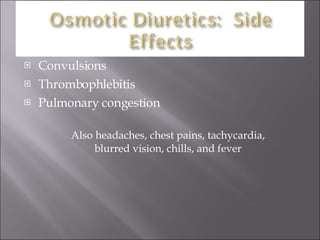
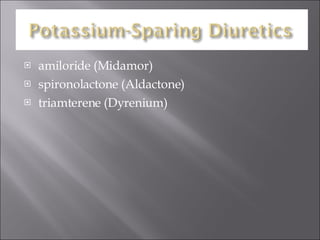
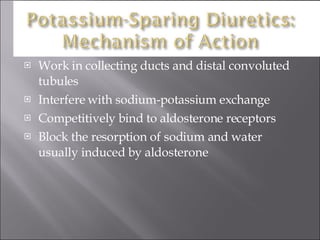
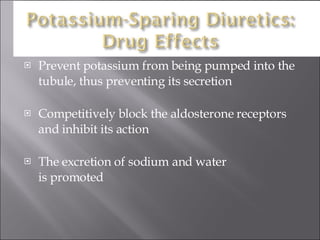
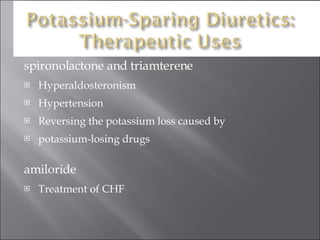
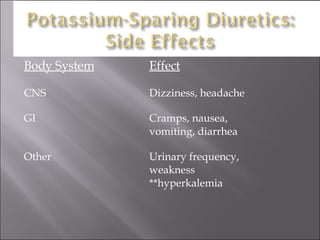
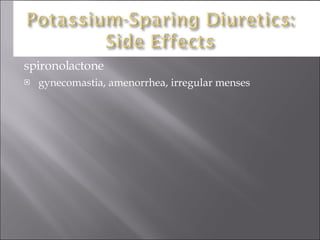
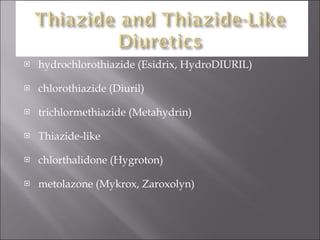
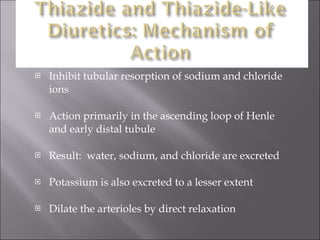
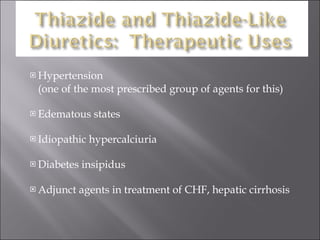
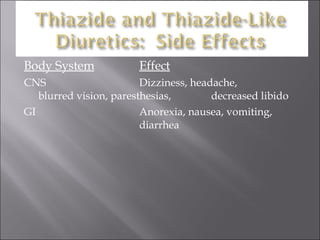
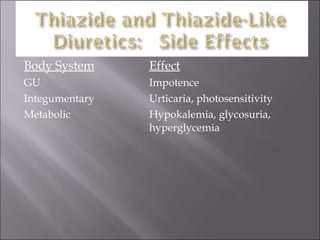
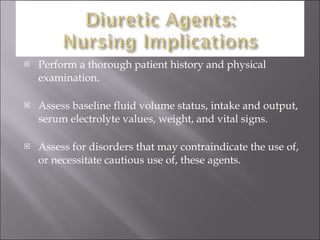
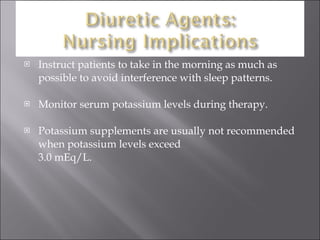
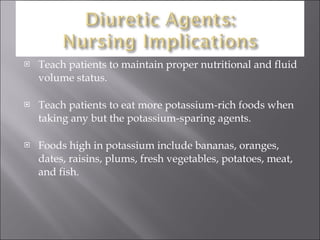
Diuretics work by increasing urine output and sodium excretion to reduce fluid overload. There are several classes of diuretics that work in different parts of the nephron: carbonic anhydrase inhibitors work in the proximal tubule; loop diuretics work in the loop of Henle; thiazides work in the distal tubule; and potassium-sparing diuretics work in the collecting ducts. Patients taking diuretics require monitoring of fluid balance and electrolytes to watch for side effects like hypokalemia and hypotension.