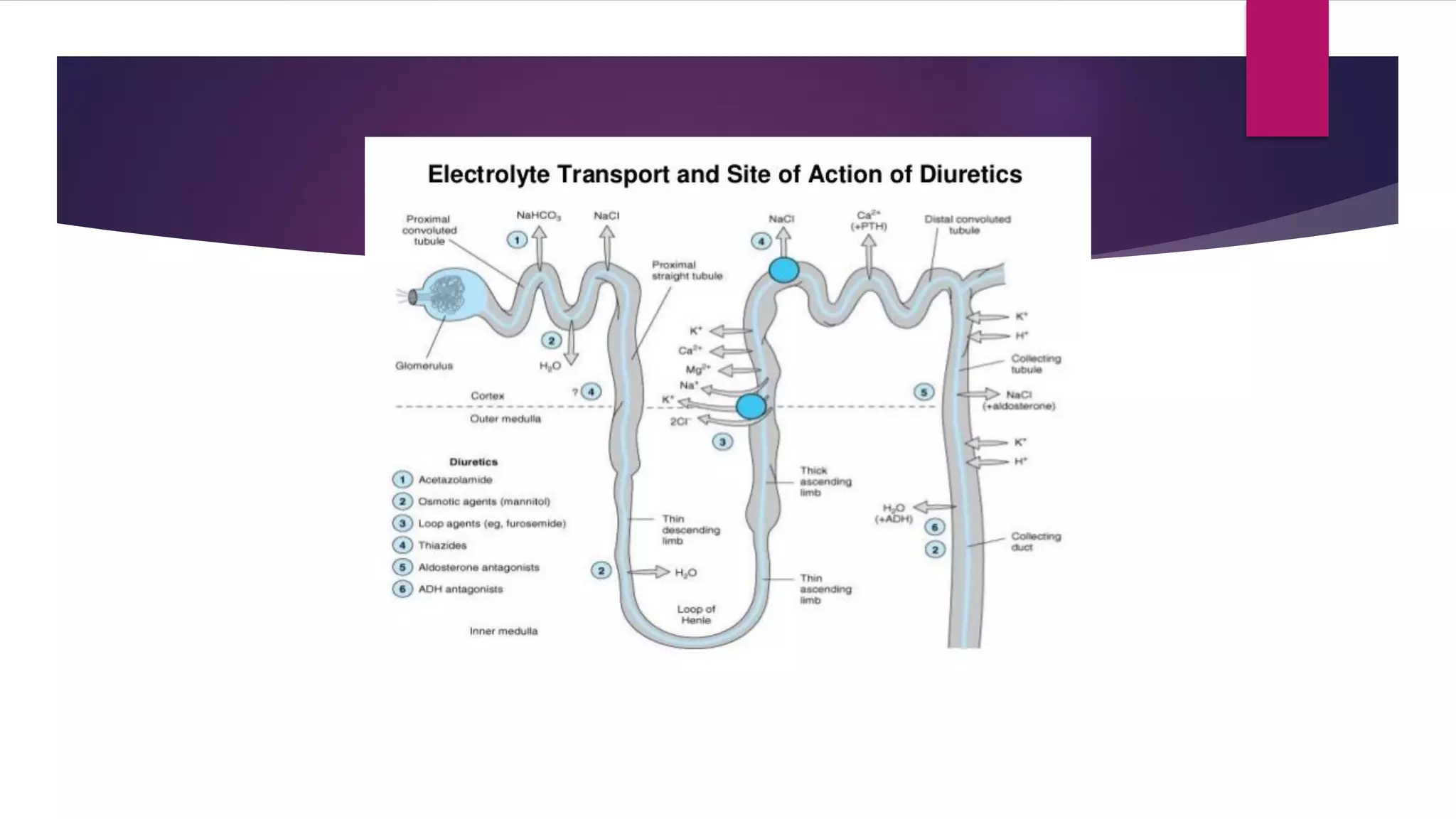
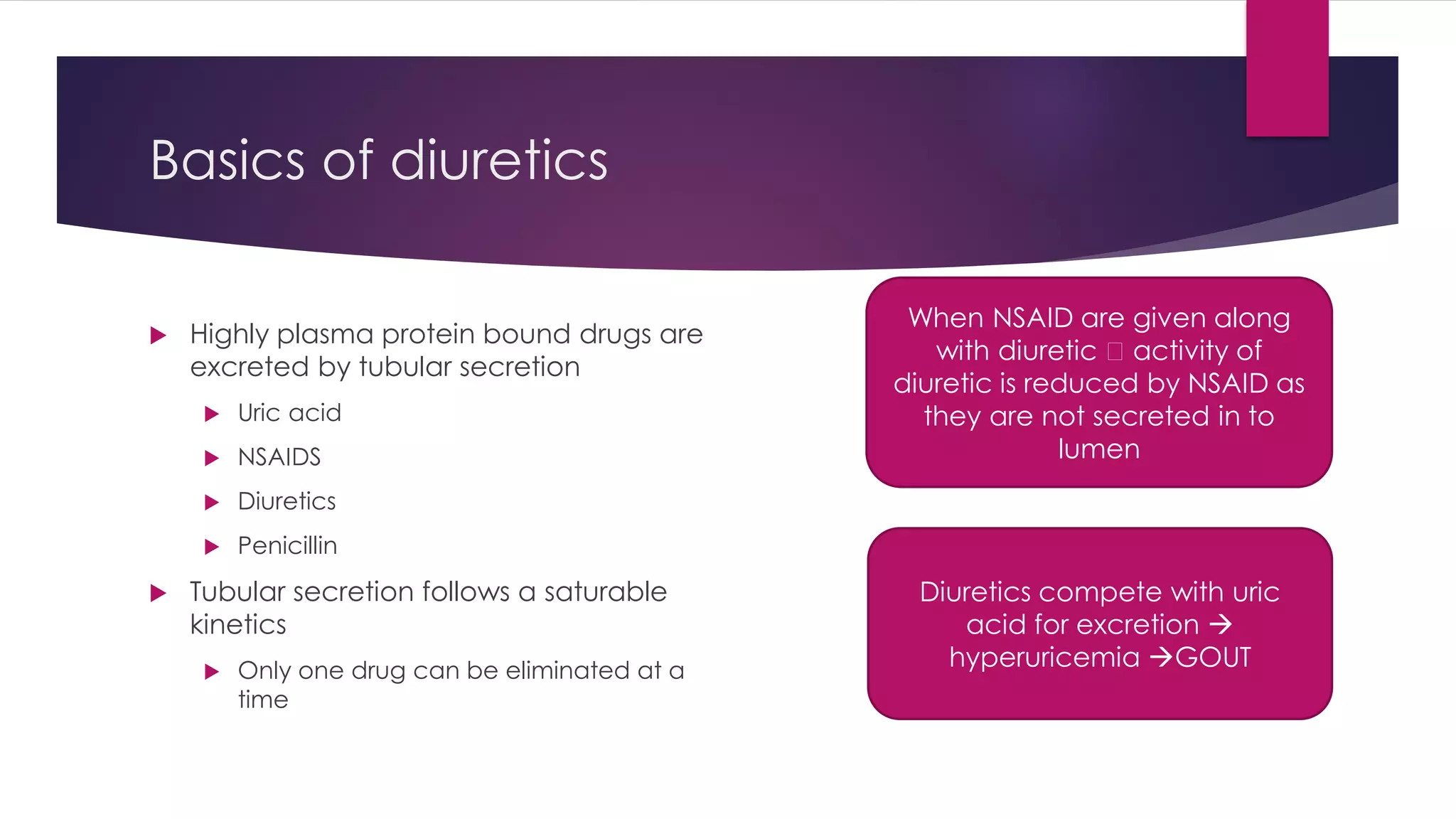
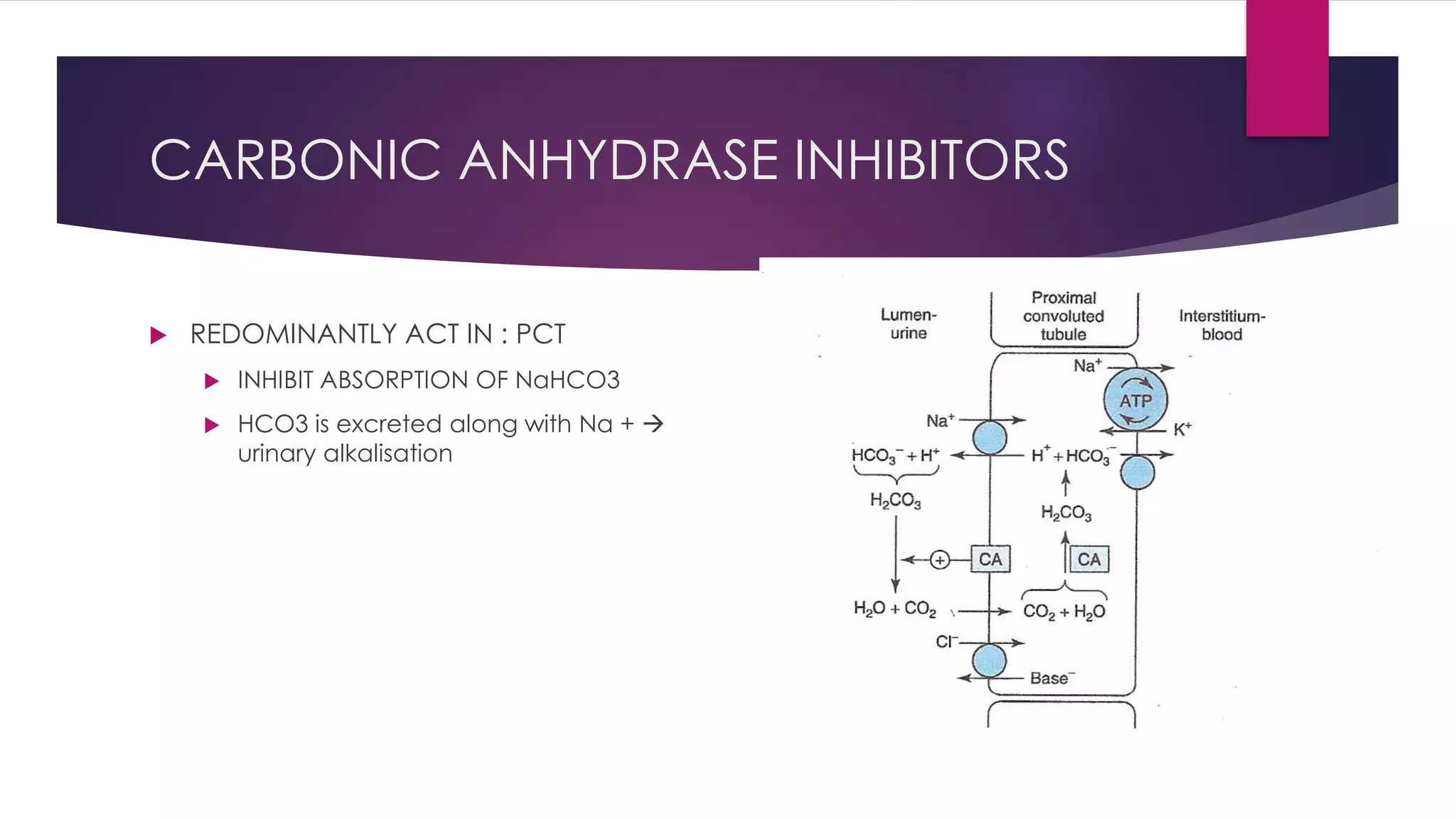
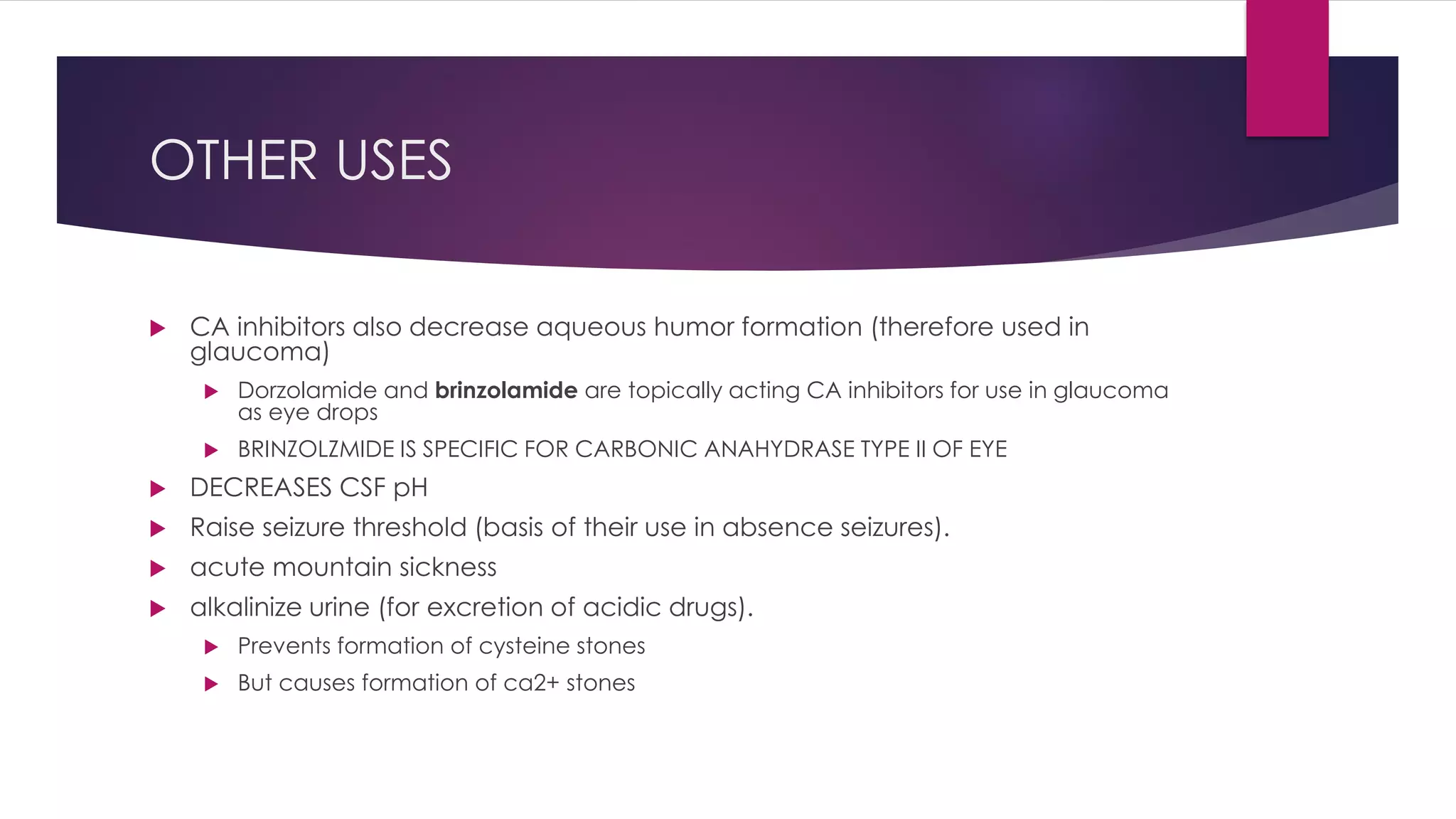
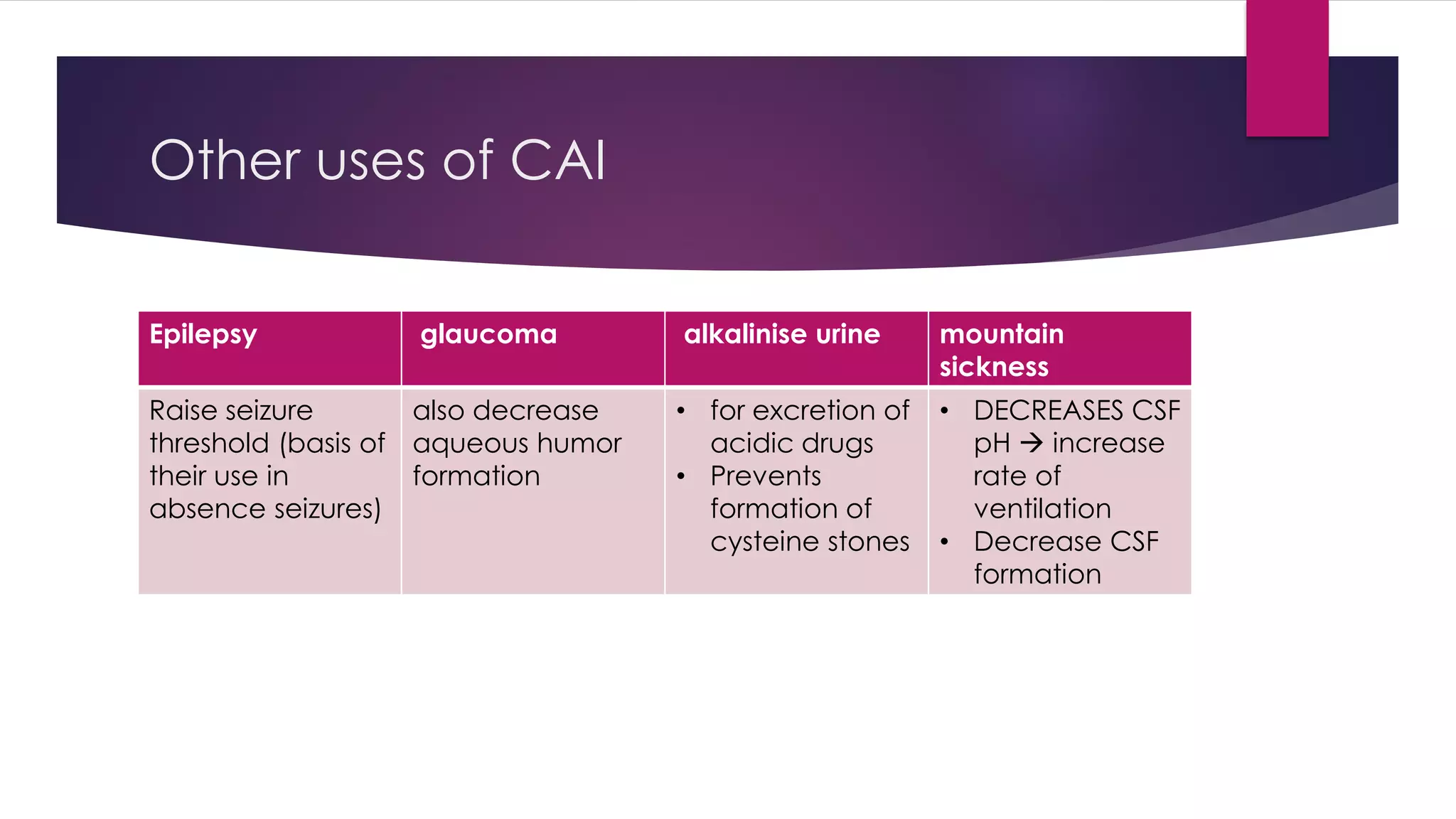
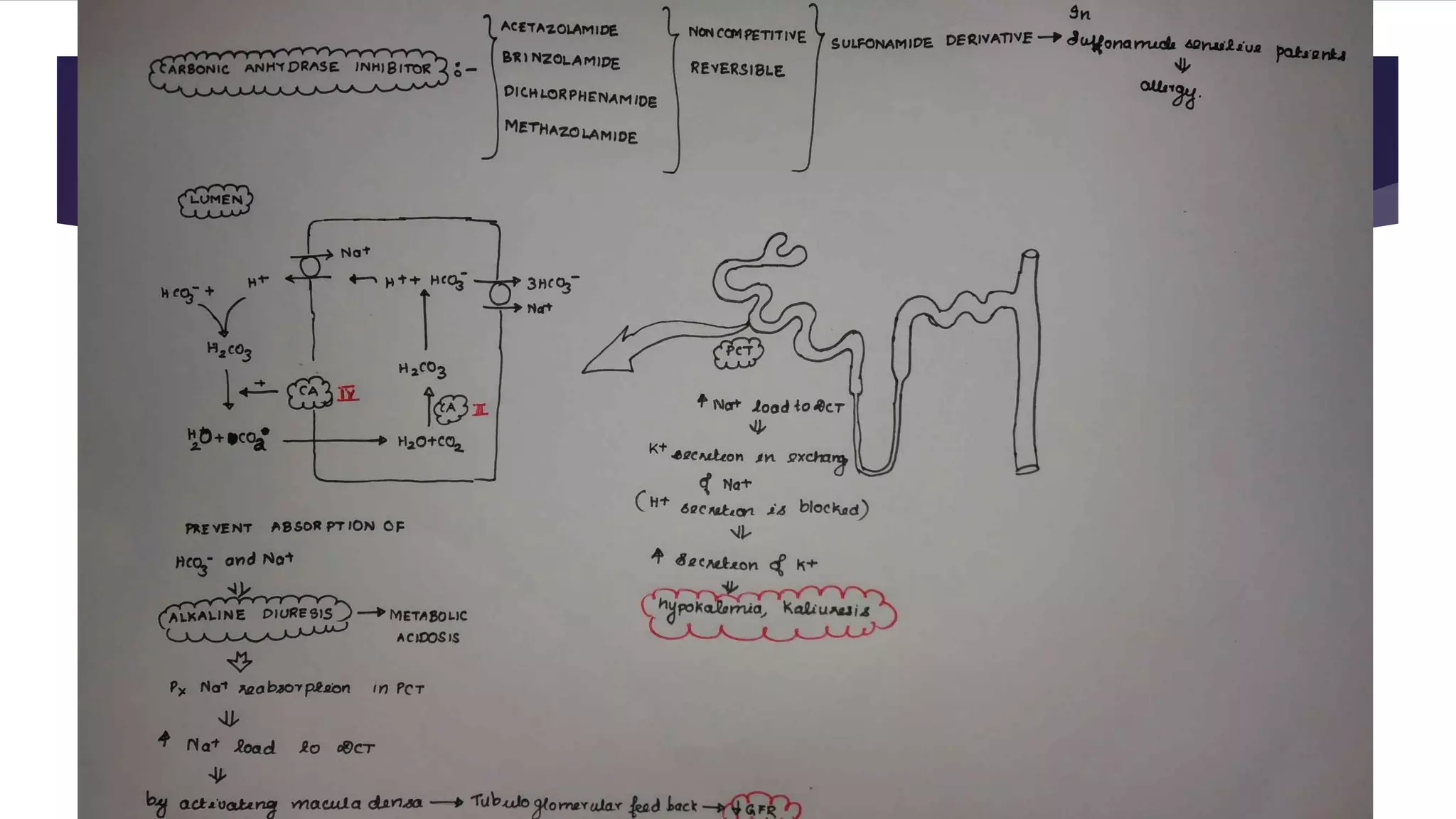
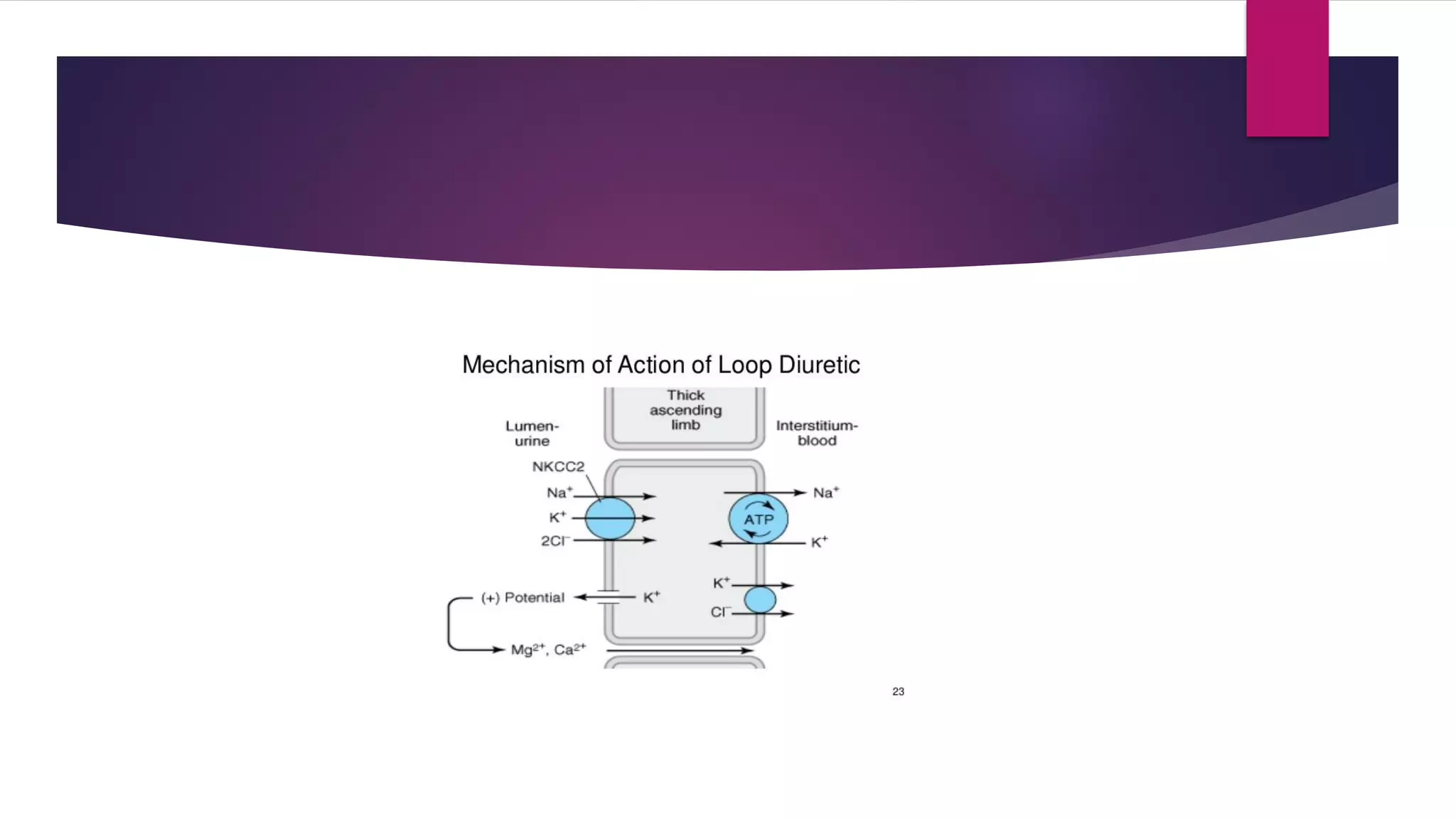
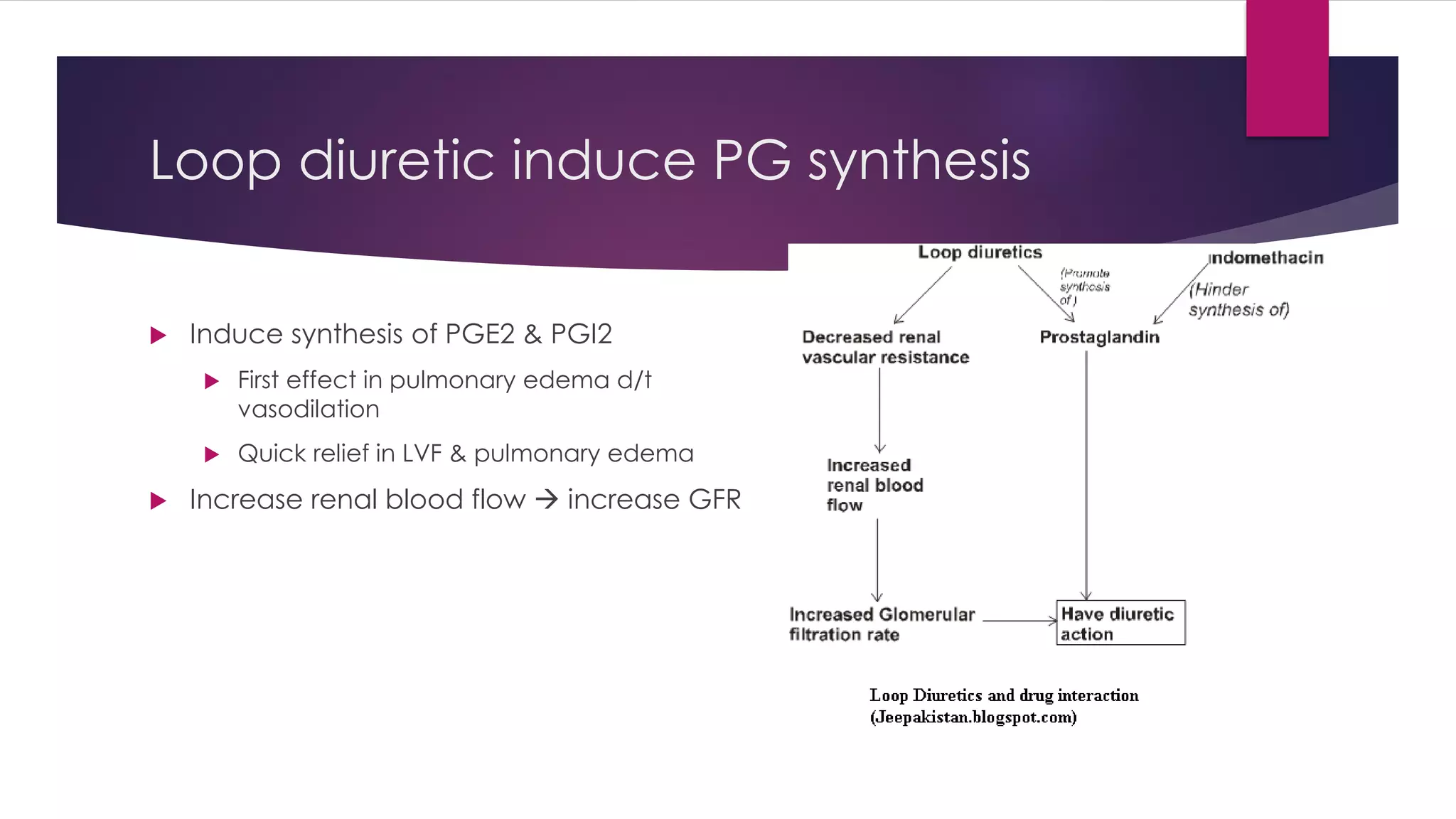
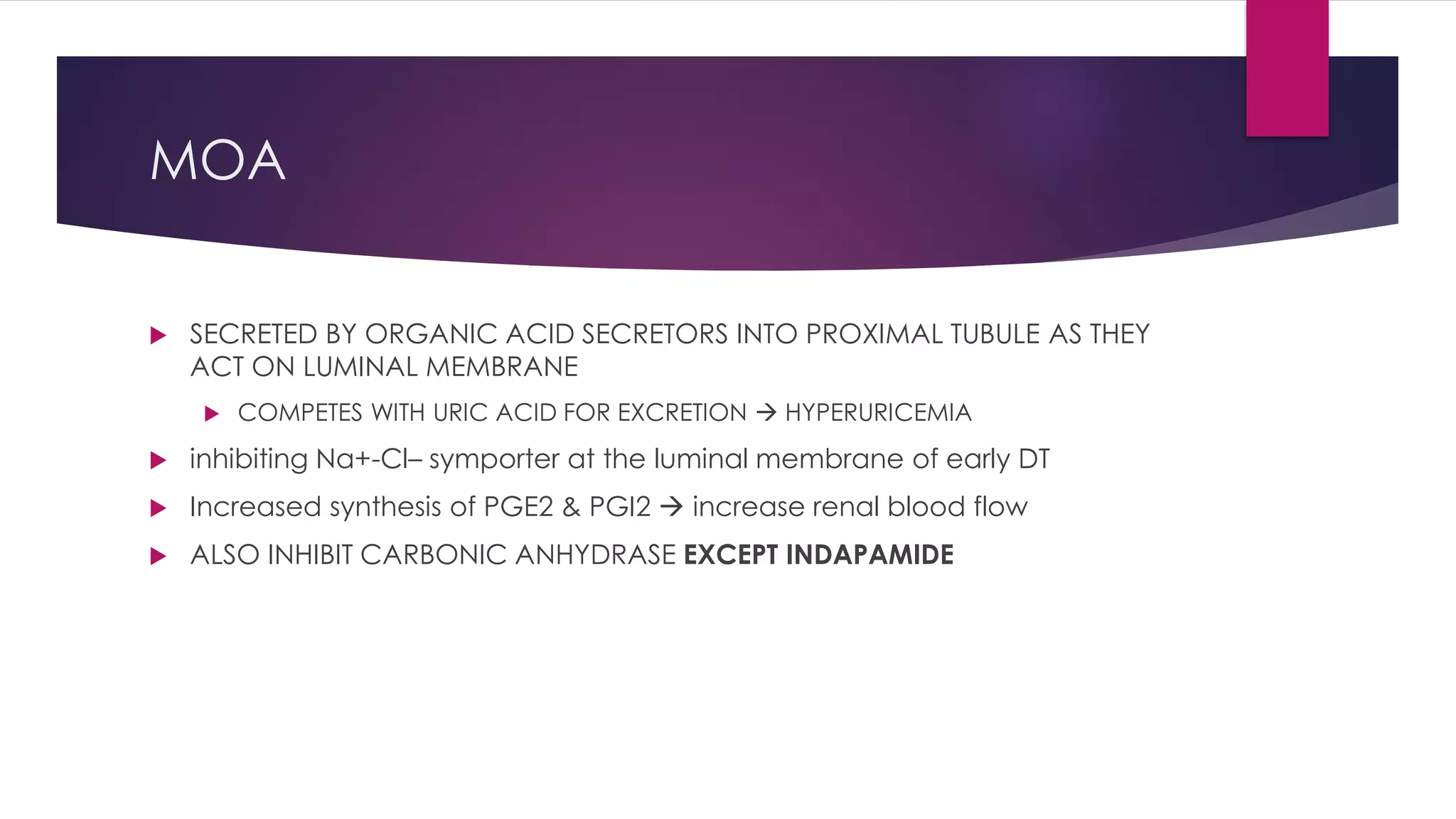
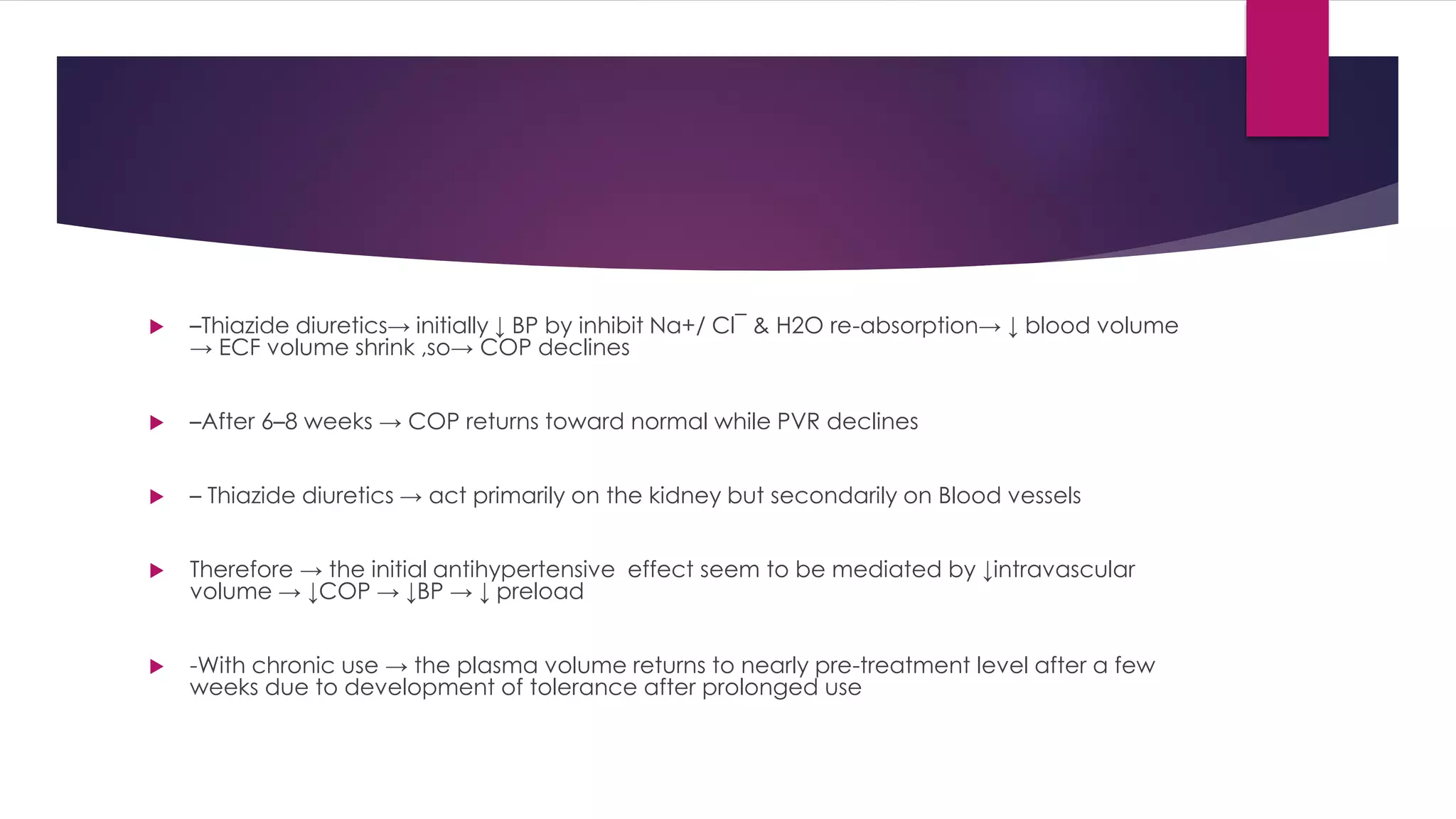
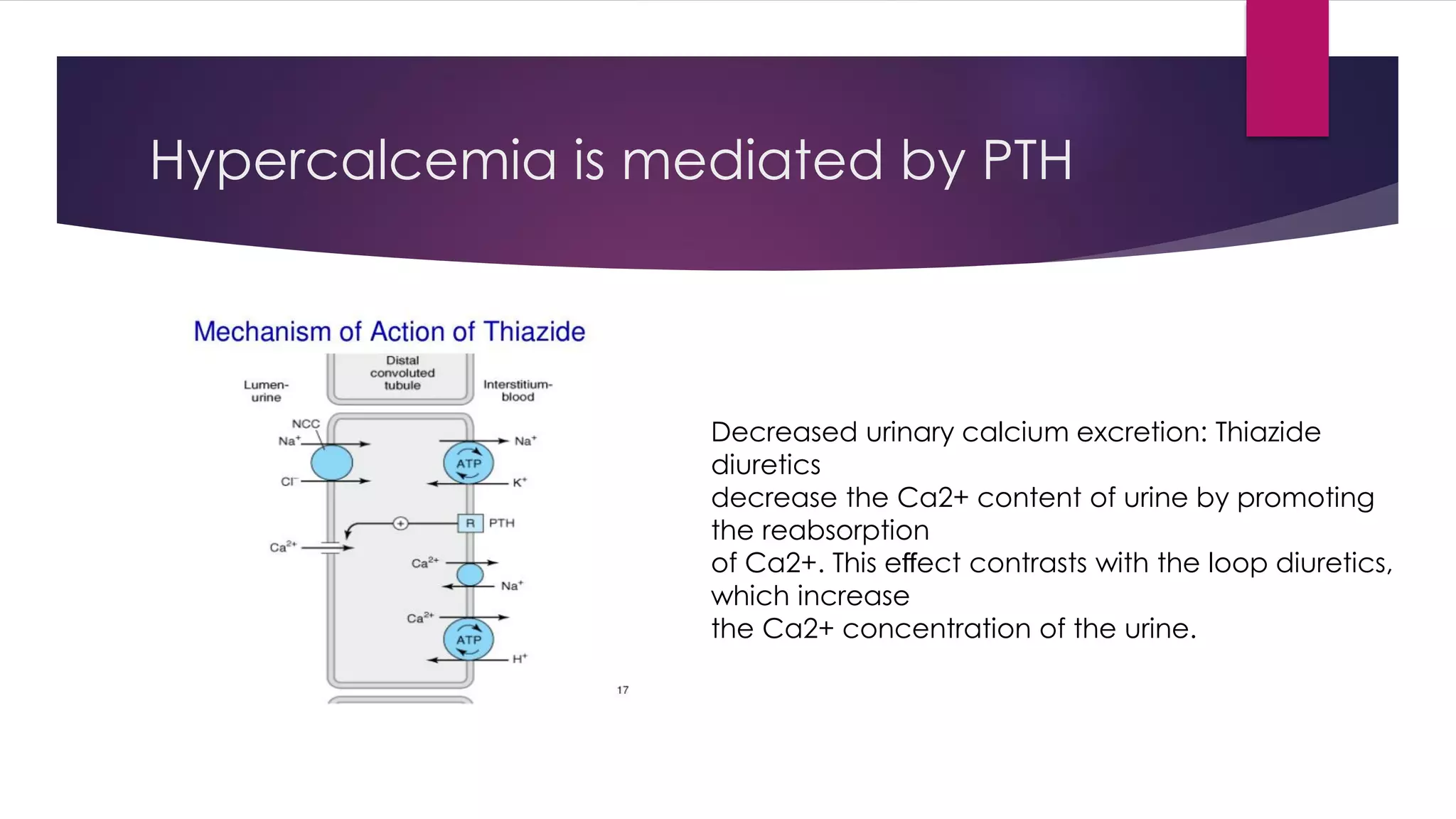
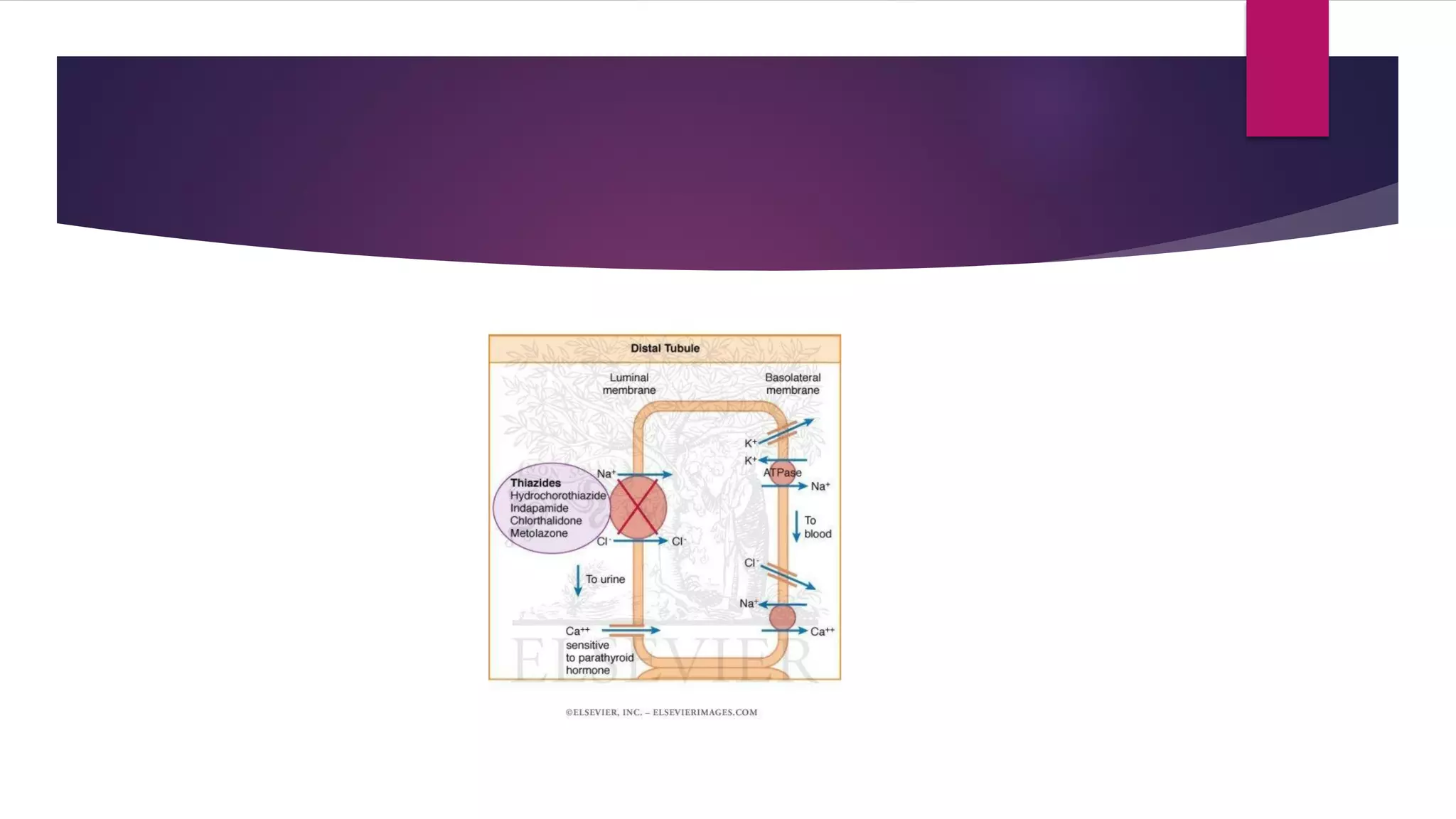
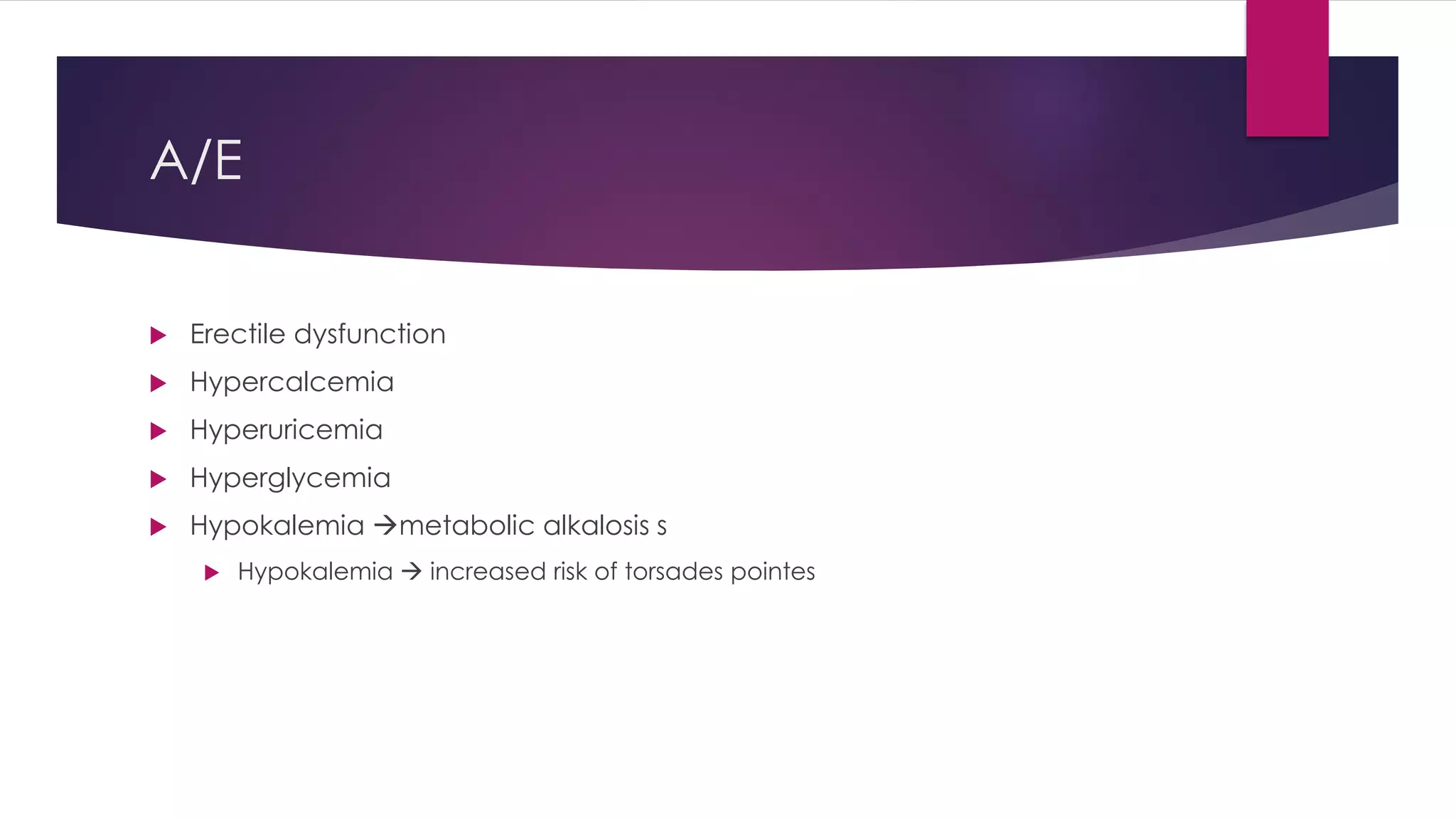
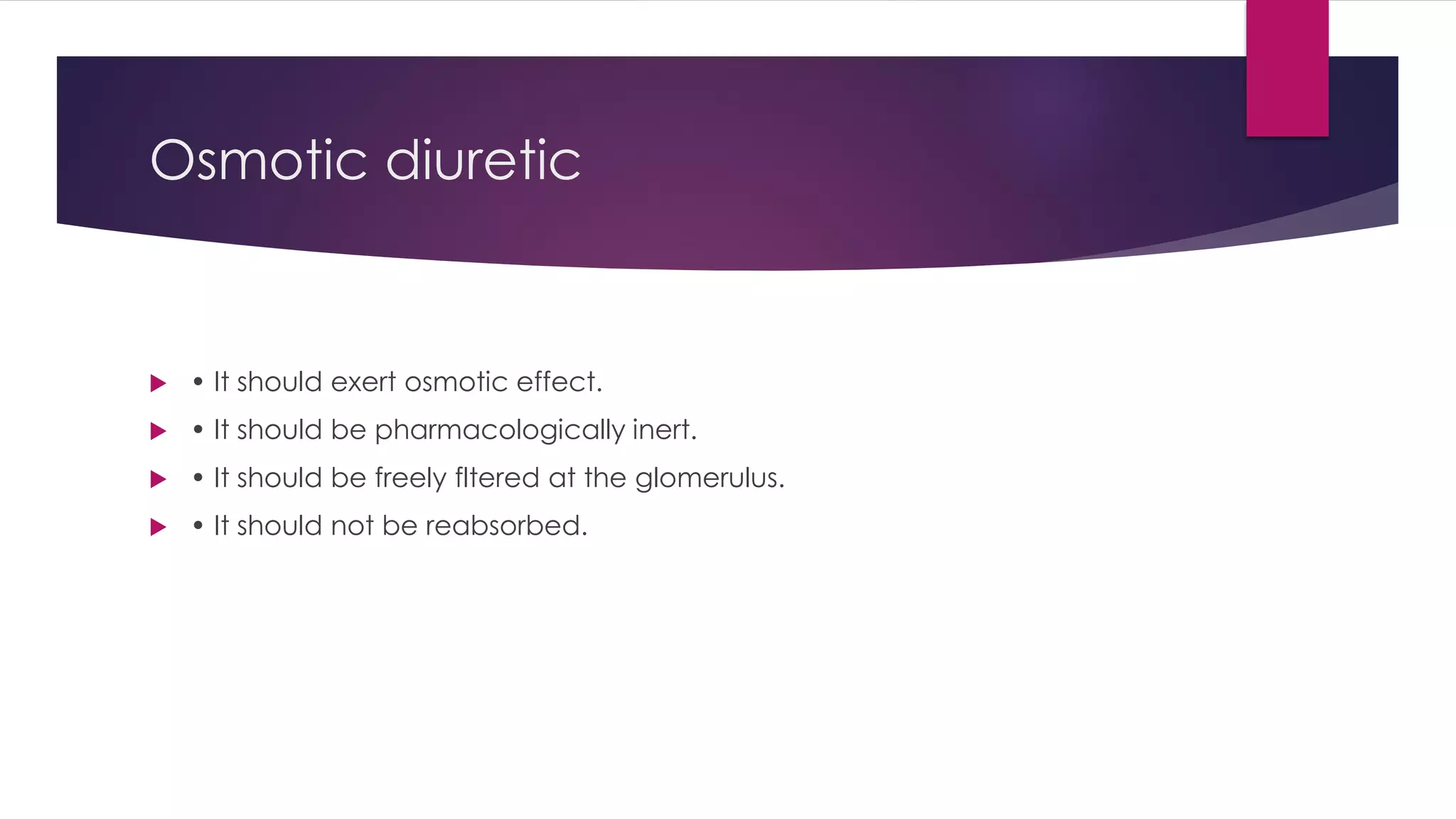
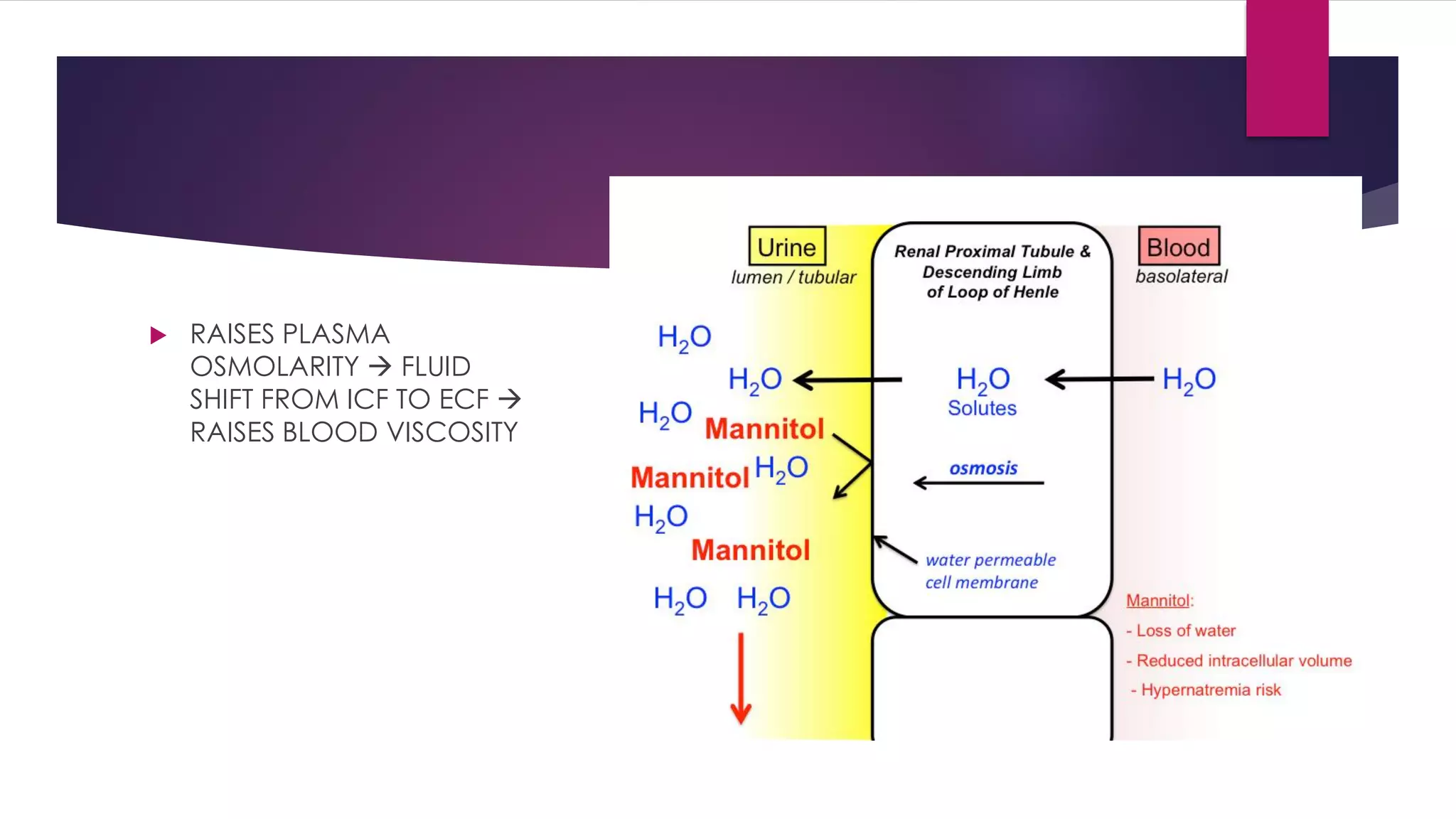
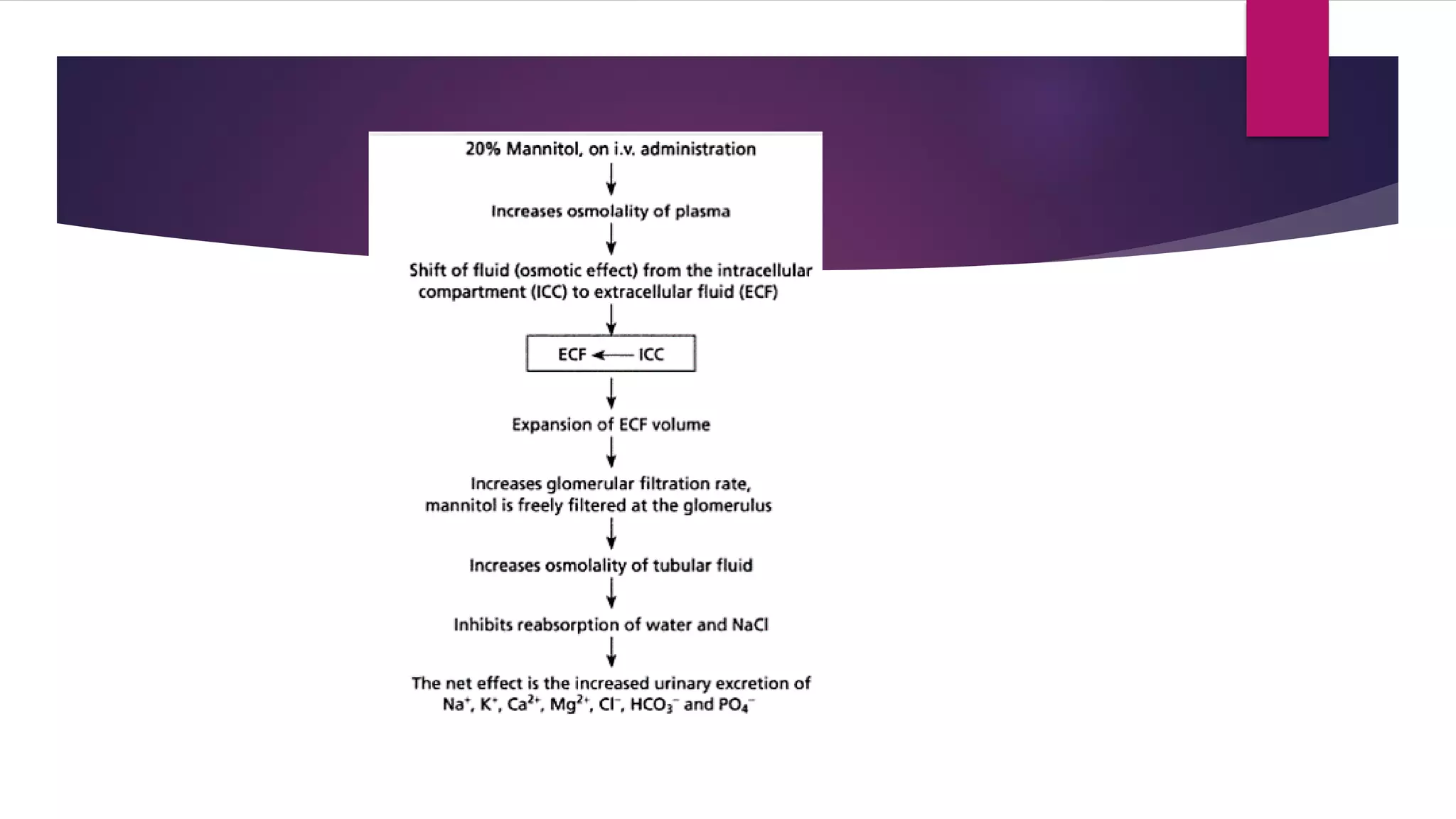
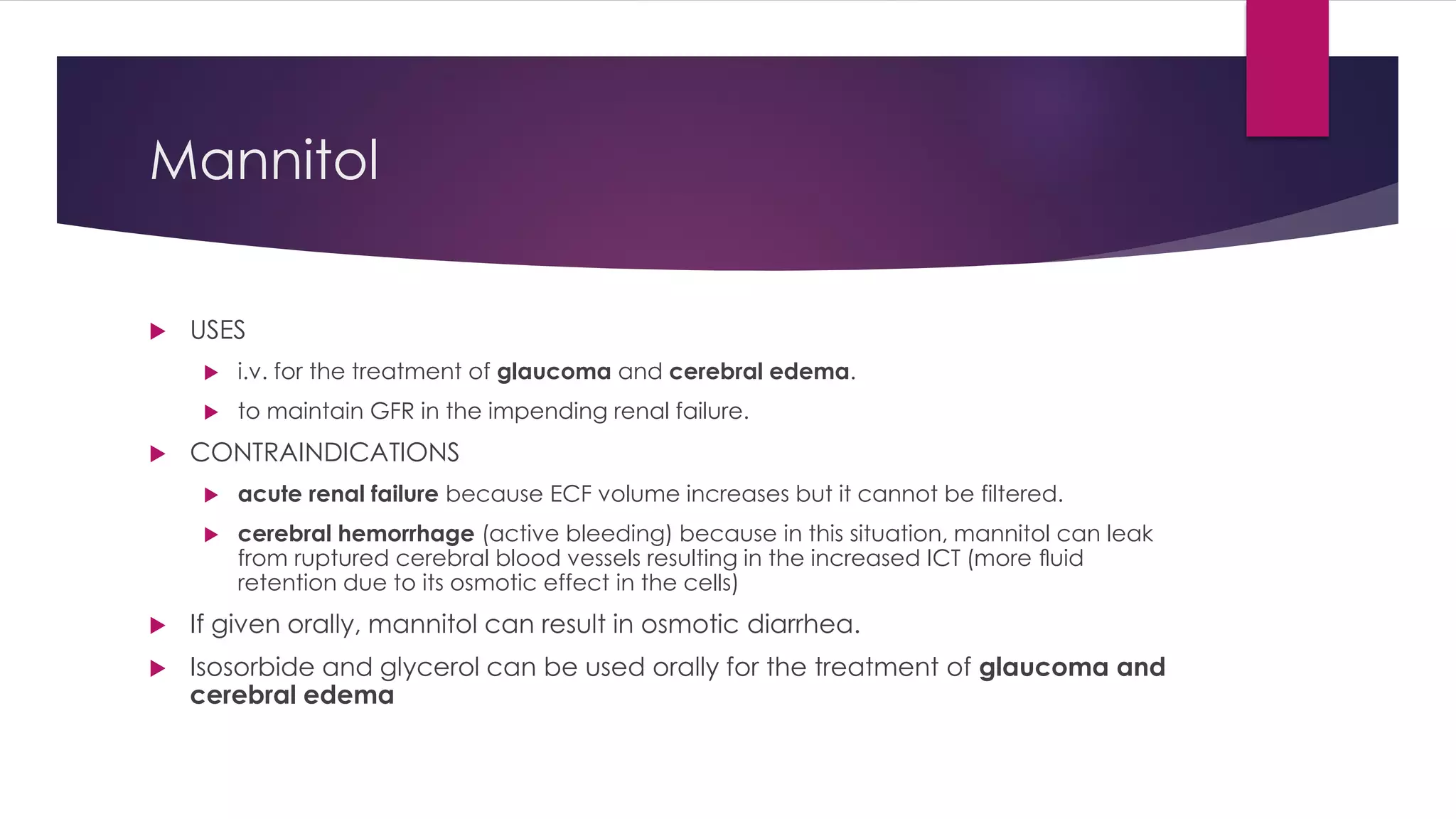
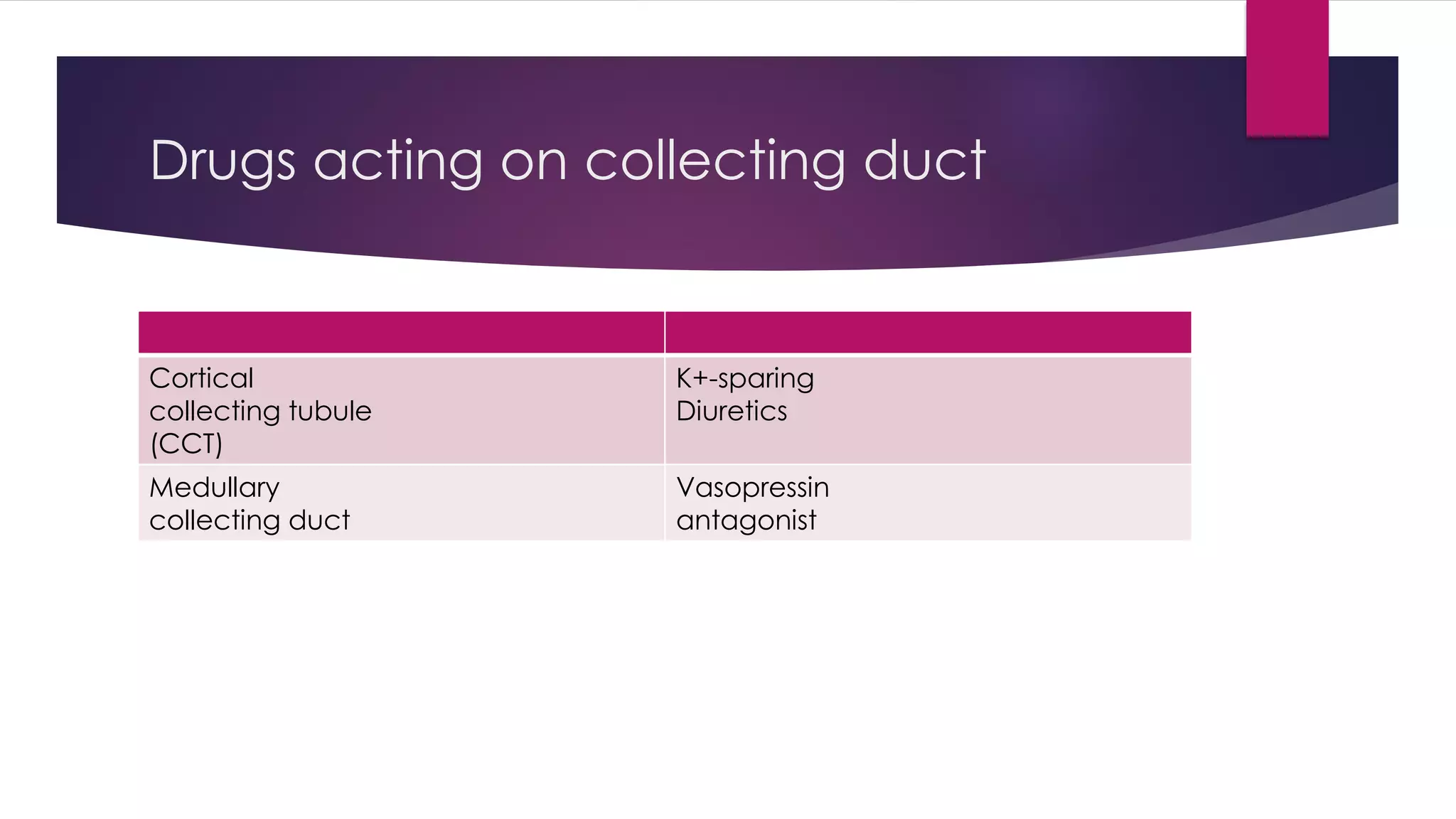
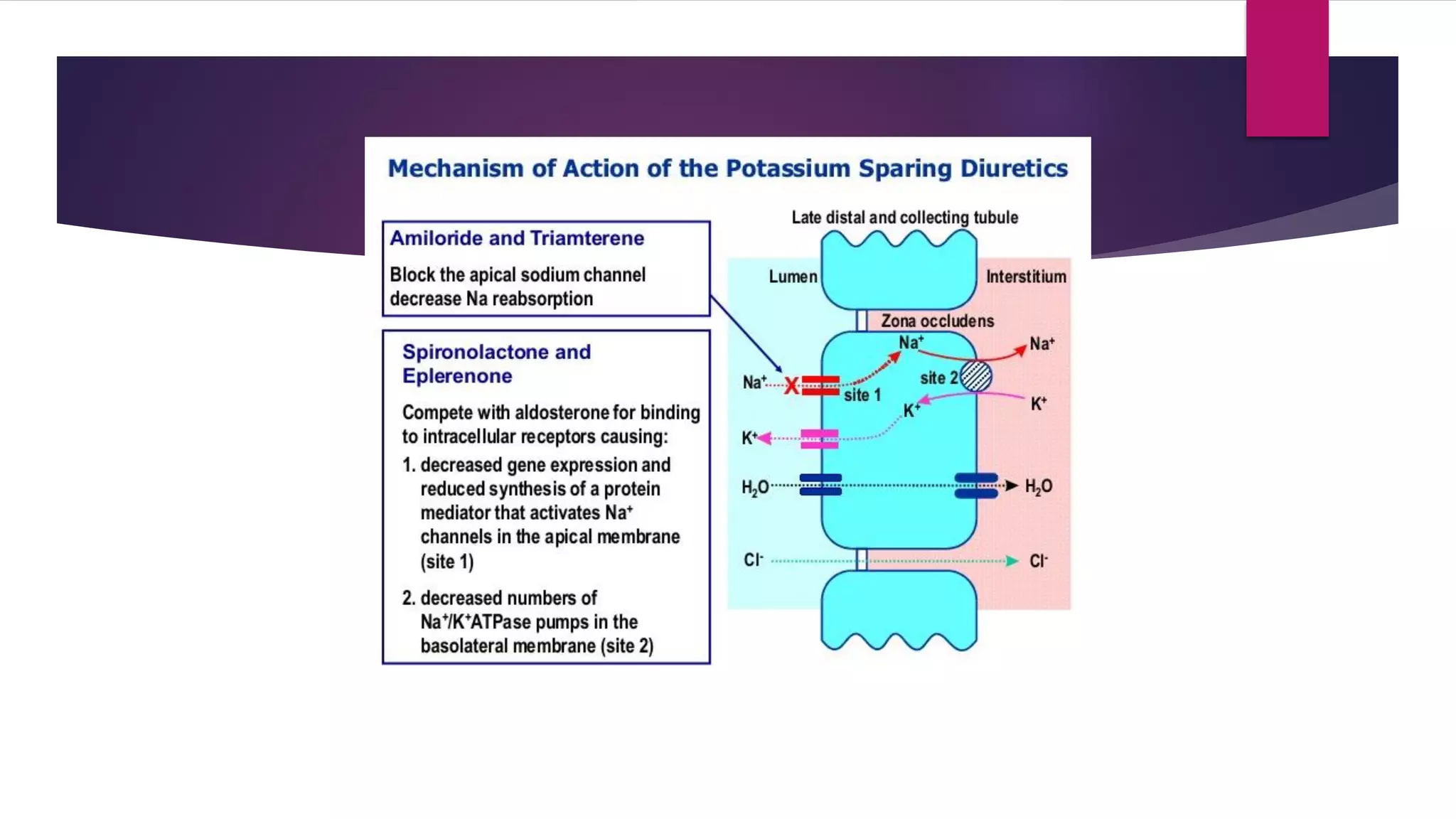
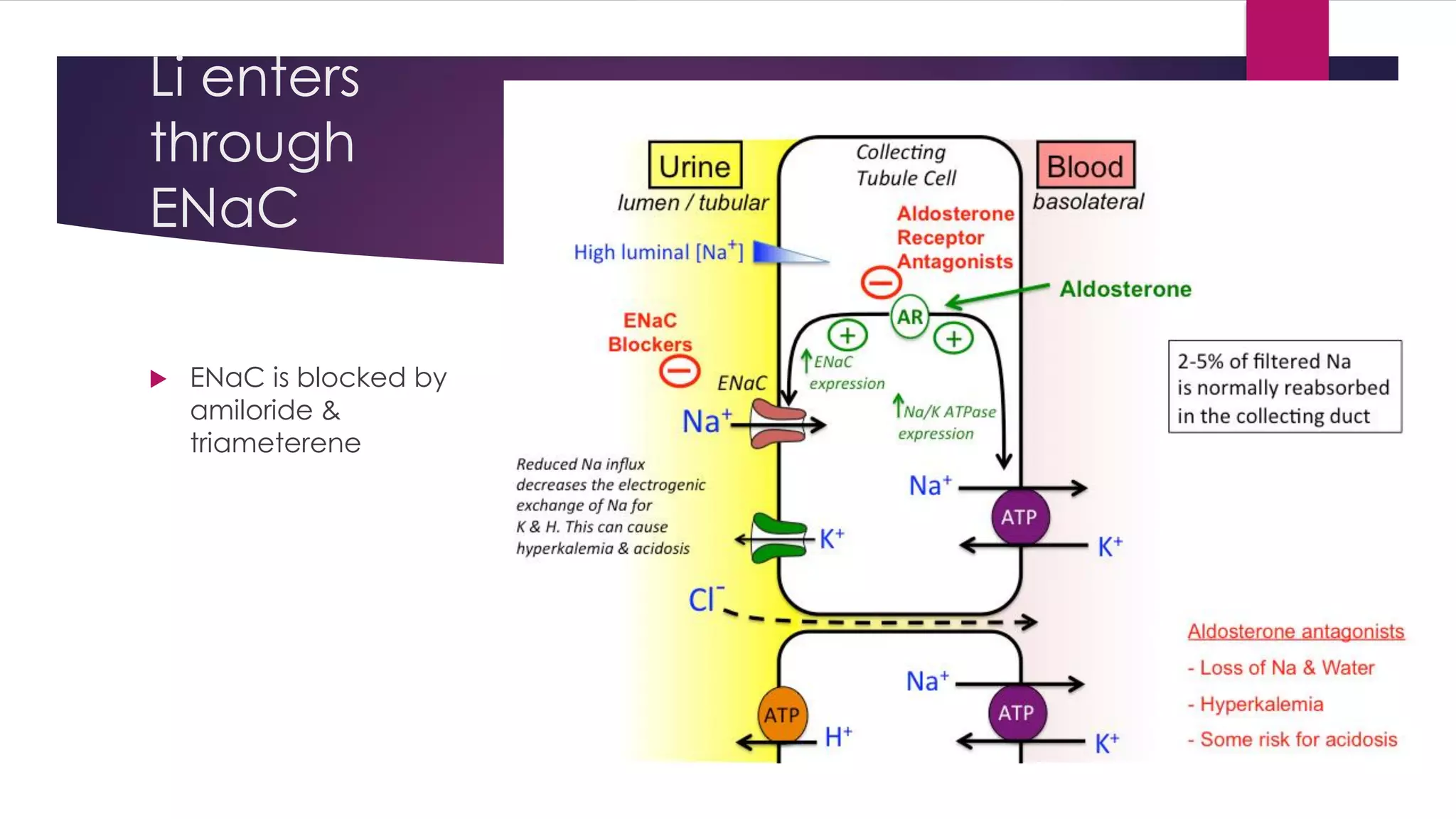
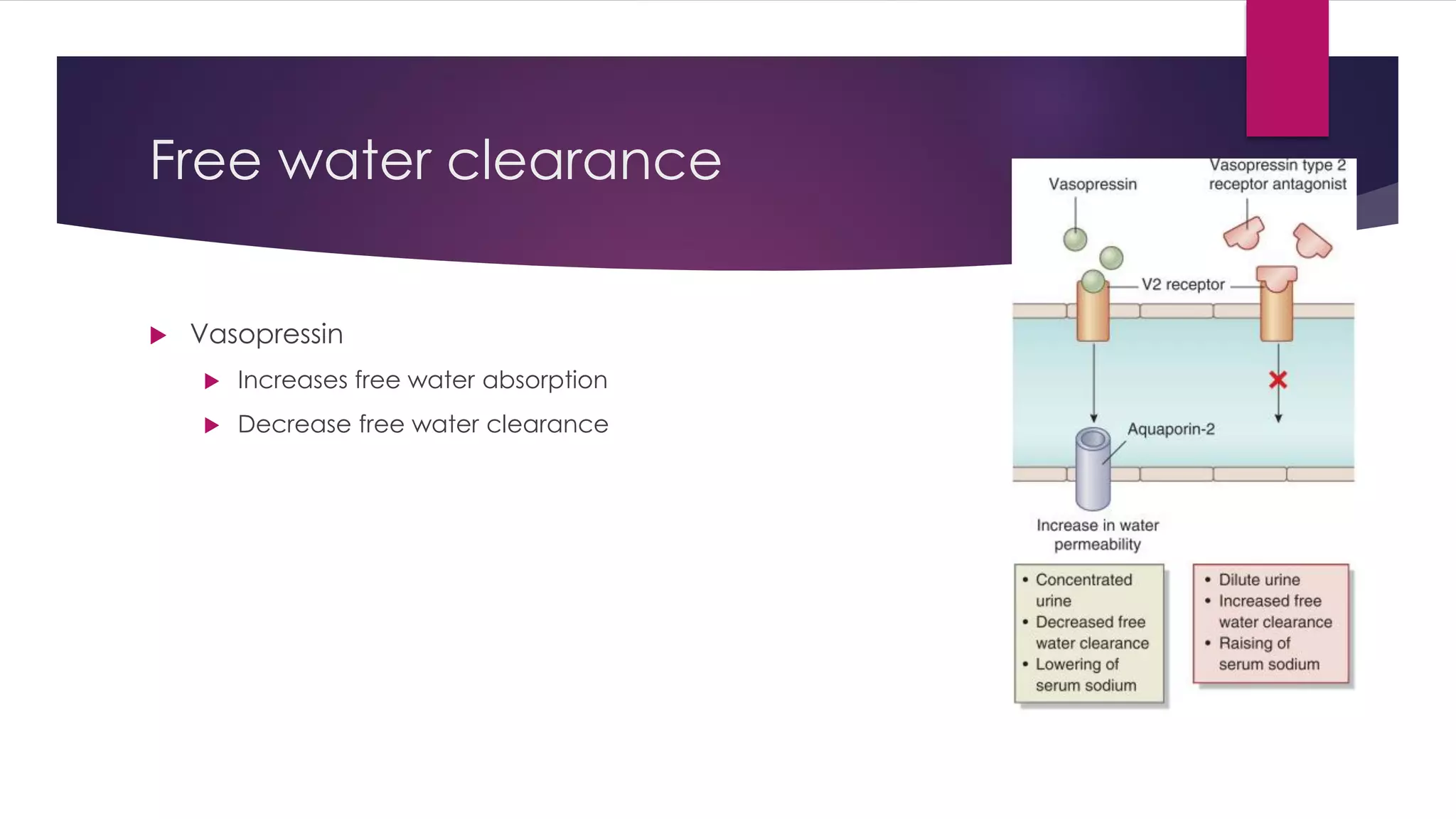
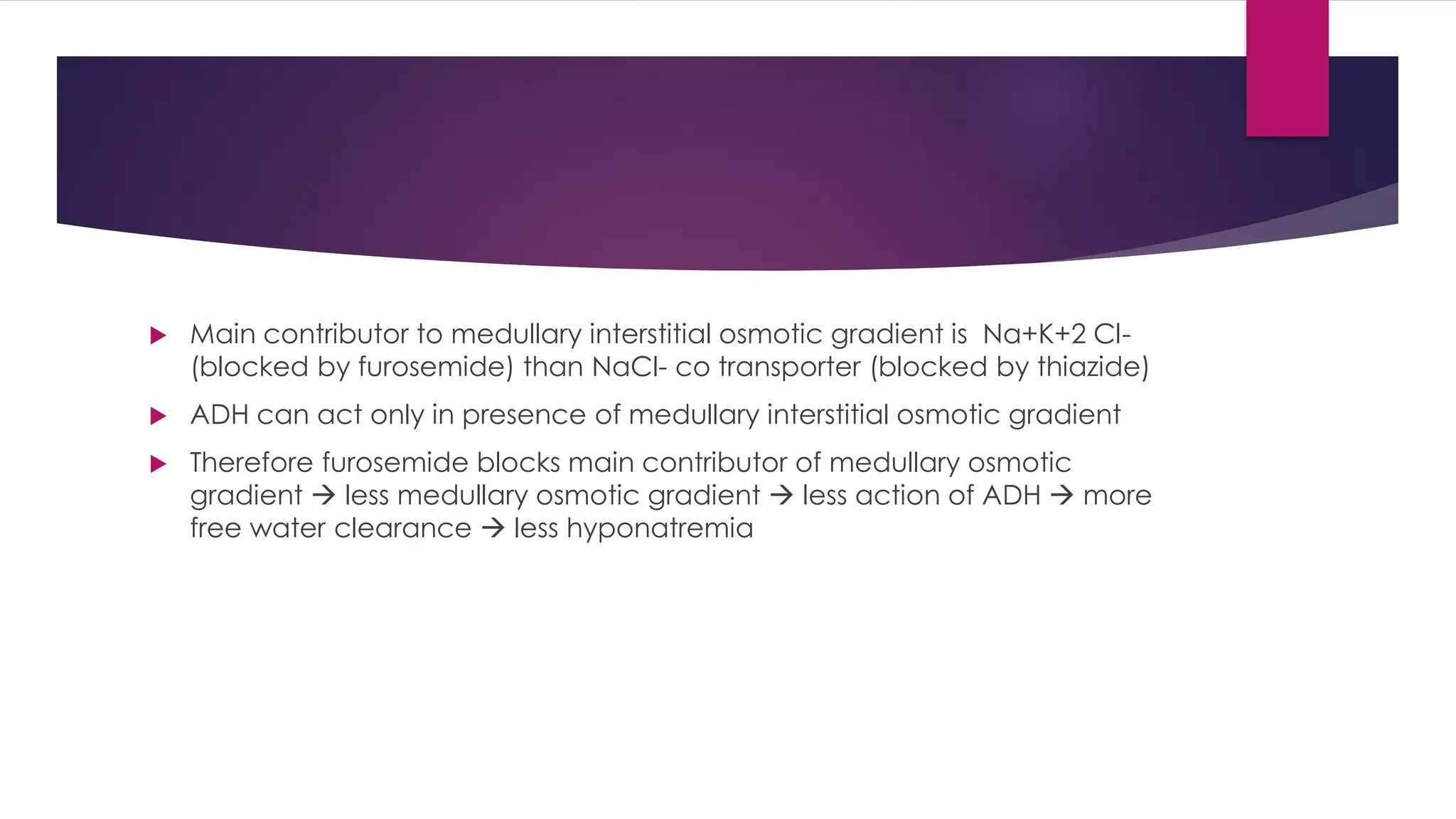
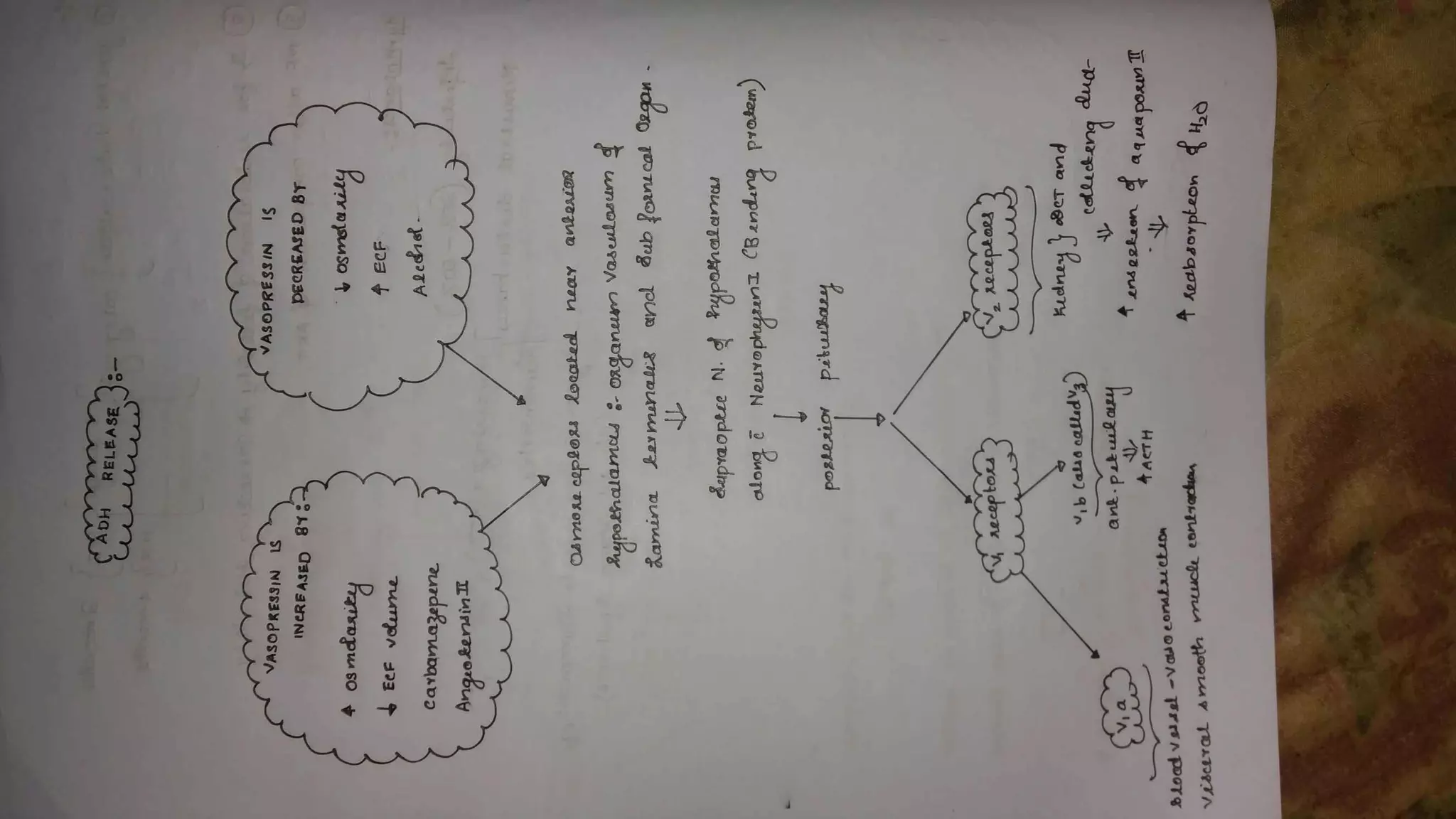
The document provides a comprehensive overview of various diuretics, including their mechanisms of action, side effects, and clinical uses. It covers categories such as carbonic anhydrase inhibitors, loop diuretics, thiazide diuretics, osmotic diuretics, and potassium-sparing diuretics, detailing their impact on renal function and electrolyte balance. Additionally, it discusses the role of diuretics in treating conditions like hypertension, heart failure, and edema, alongside potential adverse effects and contraindications.