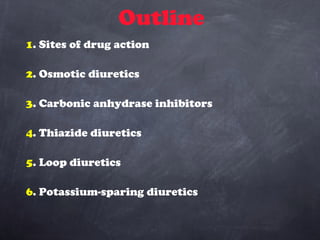
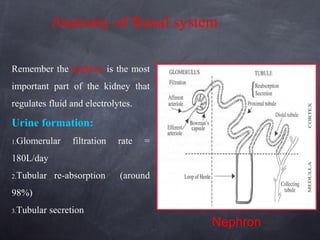
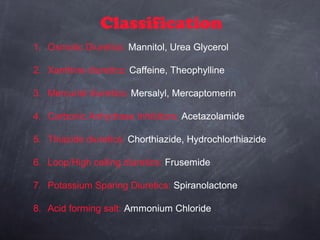
The document outlines the different classes of diuretics, their mechanisms of action, therapeutic uses, and associated side effects. It details osmotic, xanthine, carbonic anhydrase inhibitors, thiazide, loop, and potassium-sparing diuretics, emphasizing their role in conditions such as hypertension, edema, and renal failure. It also discusses the renal physiology involved in urine formation and the significance of nephron function.









![Mechanism of Action
inhibits carbonic anhydrase in renal proximal tubule cells
carbonic anhydrase catalyzes formation of HCO3- and H+ from
H2O and CO2
inhibition of carbonic anhydrase decreases [H+] in tubule lumen
less H+ for Na+/H+
exchange
increased lumen Na+,
increased H2O
retention
Site I](https://image.slidesharecdn.com/diuretics-181226085042/85/Diuretics-16-320.jpg)
![Therapeutic Uses
used to treat chronic open-angle glaucoma
aqueous humor has high [HCO3-]
acute mountain sickness
prevention and treatment
metabolic alkalosis
sometimes epilepsy
mostly used in combination with other diuretics in
resistant patients](https://image.slidesharecdn.com/diuretics-181226085042/85/Diuretics-17-320.jpg)











![Side Effects
hyperkalemia: monitor plasma [K+]
spironolactone: gynecomastia
triamterene: megaloblastic anemia in cirrhosis
patients
amiloride: increase in blood urea nitrogen, glucose
intolerance in diabetes mellitus](https://image.slidesharecdn.com/diuretics-181226085042/85/Diuretics-33-320.jpg)