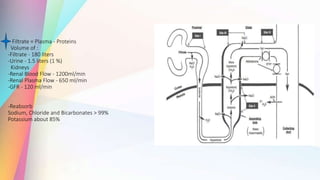
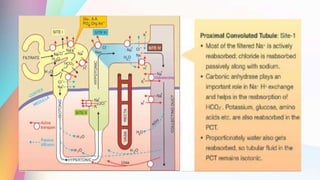
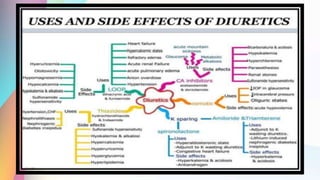
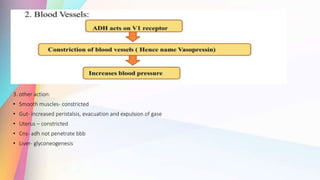
This document details diuretics and antidiuretics, defining their functions and classifications. Diuretics are drugs promoting sodium and water loss in urine, portrayed as effective treatments for various conditions like heart failure and hypertension. The document categorizes diuretics based on their site of action, efficacy, and includes pharmacokinetics and therapeutic uses of specific types, alongside relevant physiological insights about urine formation.











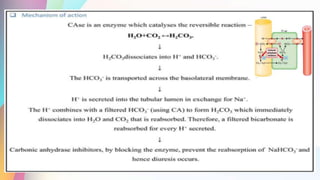

![Therapeutic Uses:
-Used to treat chronic open-angle glaucoma
-High aqueous humor [HCO3-] acute mountain sickness
- Prevention and treatment metabolic alkalosis
-Mostly used in combination with other diuretics in resistant patients.
Side Effects:
-Rapid tolerance
-Increased HCO3- excretion causes metabolic acidosis
-Drowsiness
-Fatigue
-CNS depression
-Paresthesia (pins and needles under skin)
-Nephrolithiasis (renal stones) K+ wasting
-hypersensitivity reaction
-skin rashes
-fever
-headache
Contraindication:
- Liver cirrhosis (CA-I inhibits conversion of NH to NH4) -> NH3 increased encephalopathy
-copd: worsening of metabolic acidosis is seen in patient with chronic obstructive pulmonary disease.](https://image.slidesharecdn.com/diureticsndantidiureticsnv-231208011753-b967eda0/85/Diuretics-and-antidiuretics-detail-STUDY-20-320.jpg)














![Refrence:
• Essentials of Medical Pharmacology [7th Edition] by KD Tripathi
•Rang and Dale 8th Edition By H.P.Rang, J.M. Ritter
• Katzung B.G.: Basic and Clinical Pharmacology, Lange Medical
Publications, California.
• Pharmacology for medical graduates Third edition by Tara V
Shanbhag.
•Goodman & Gilman's The Pharmacological Basis of THERAPEUTICS](https://image.slidesharecdn.com/diureticsndantidiureticsnv-231208011753-b967eda0/85/Diuretics-and-antidiuretics-detail-STUDY-54-320.jpg)
