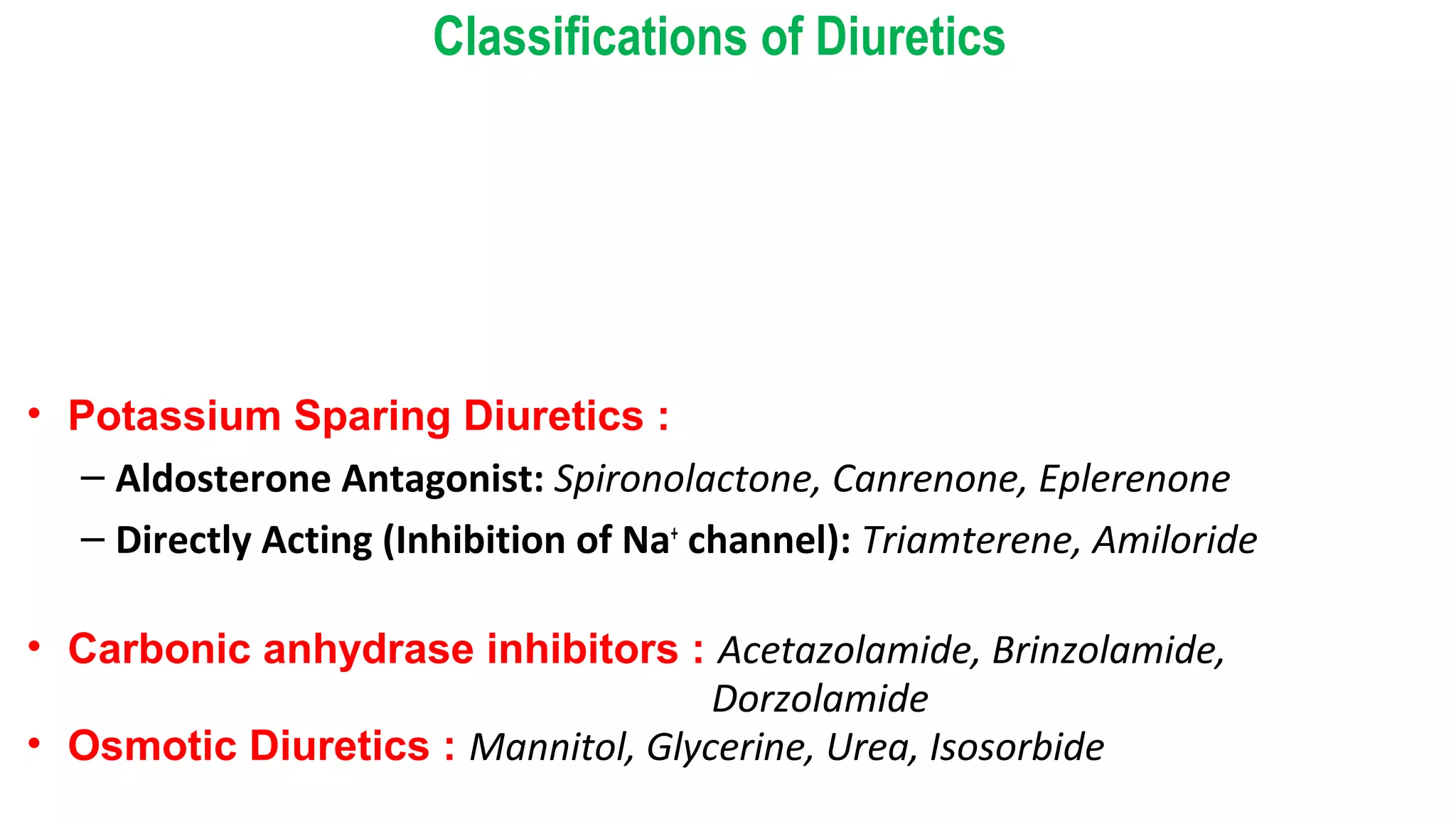
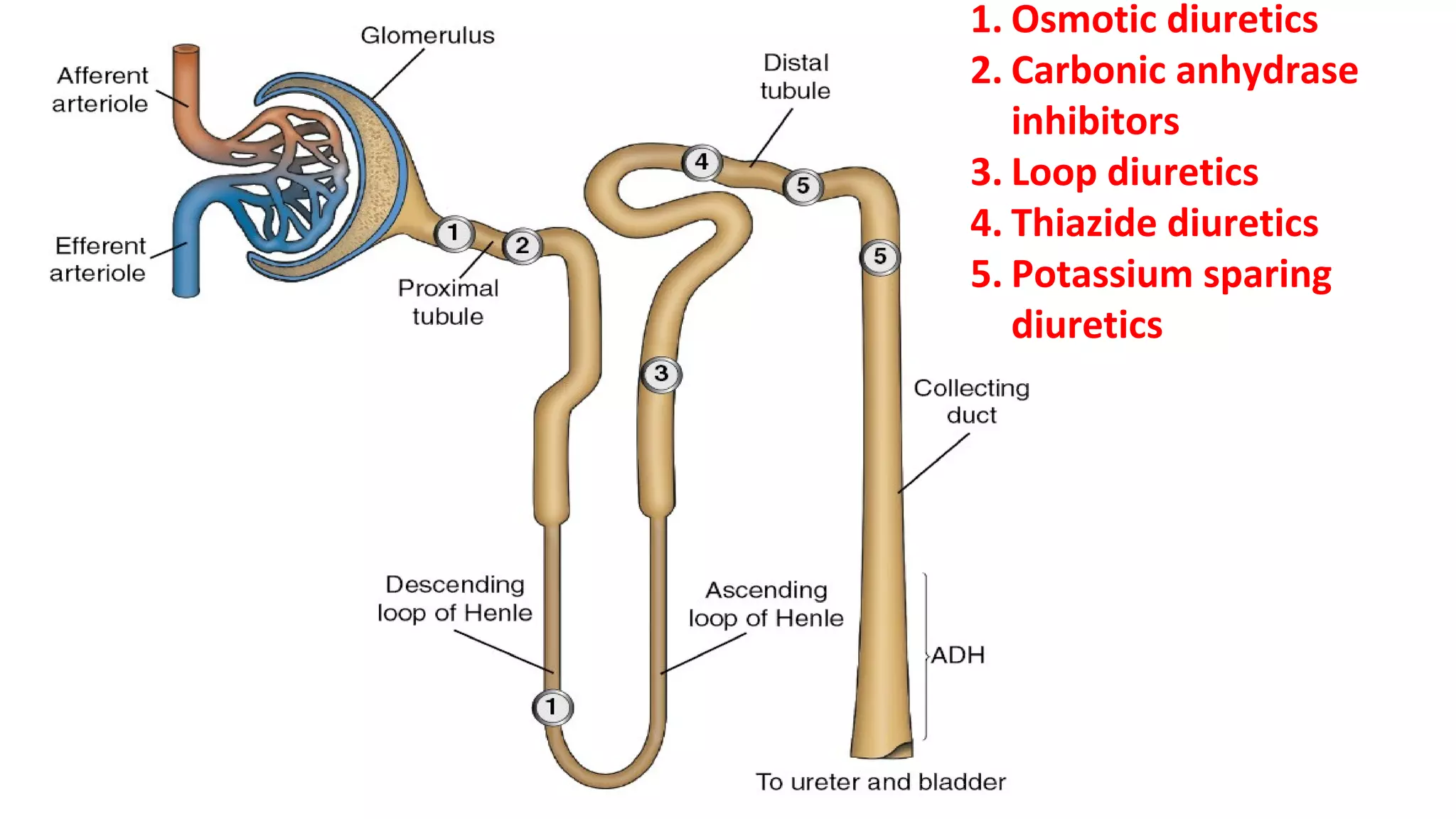
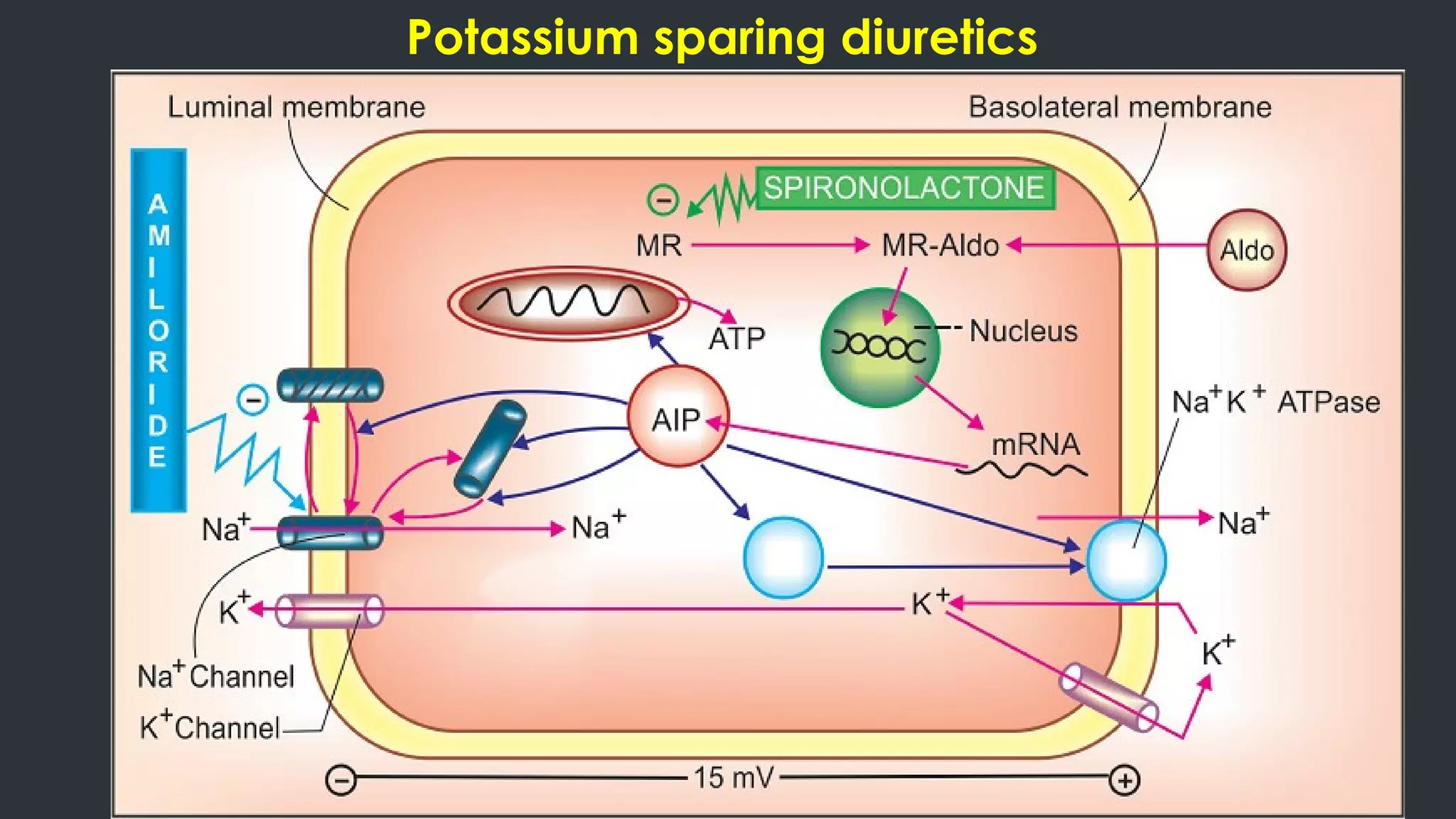
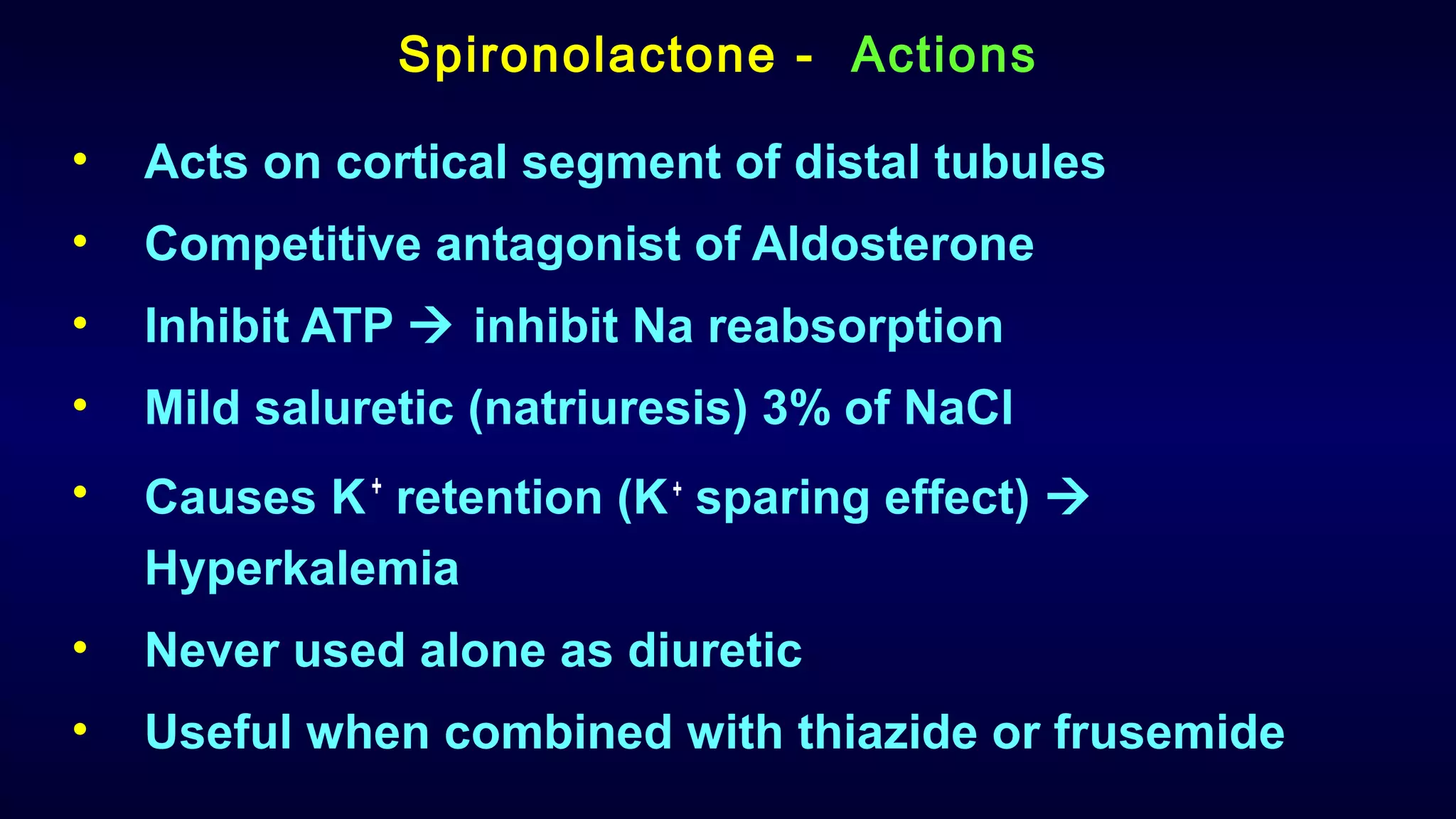
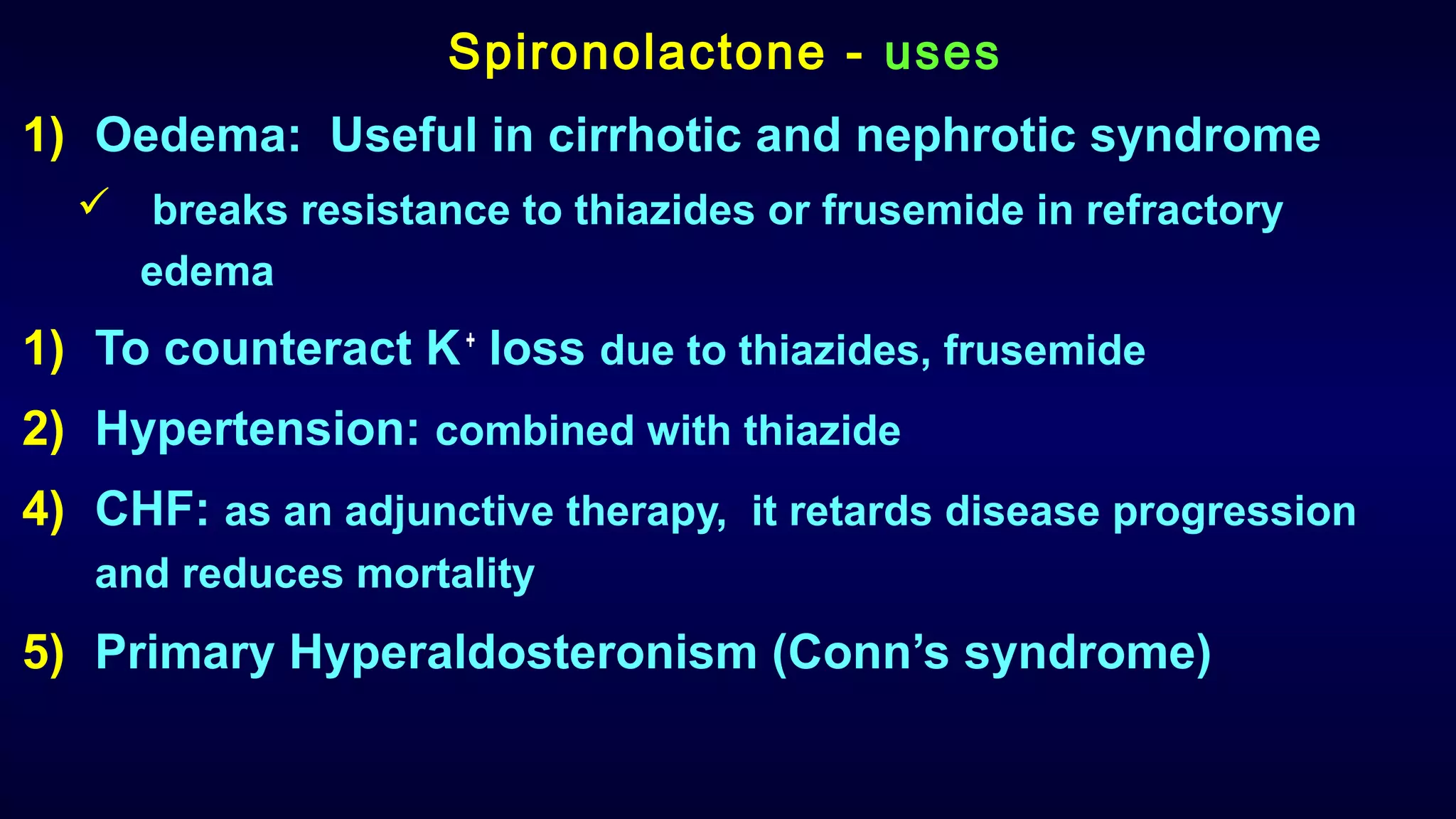
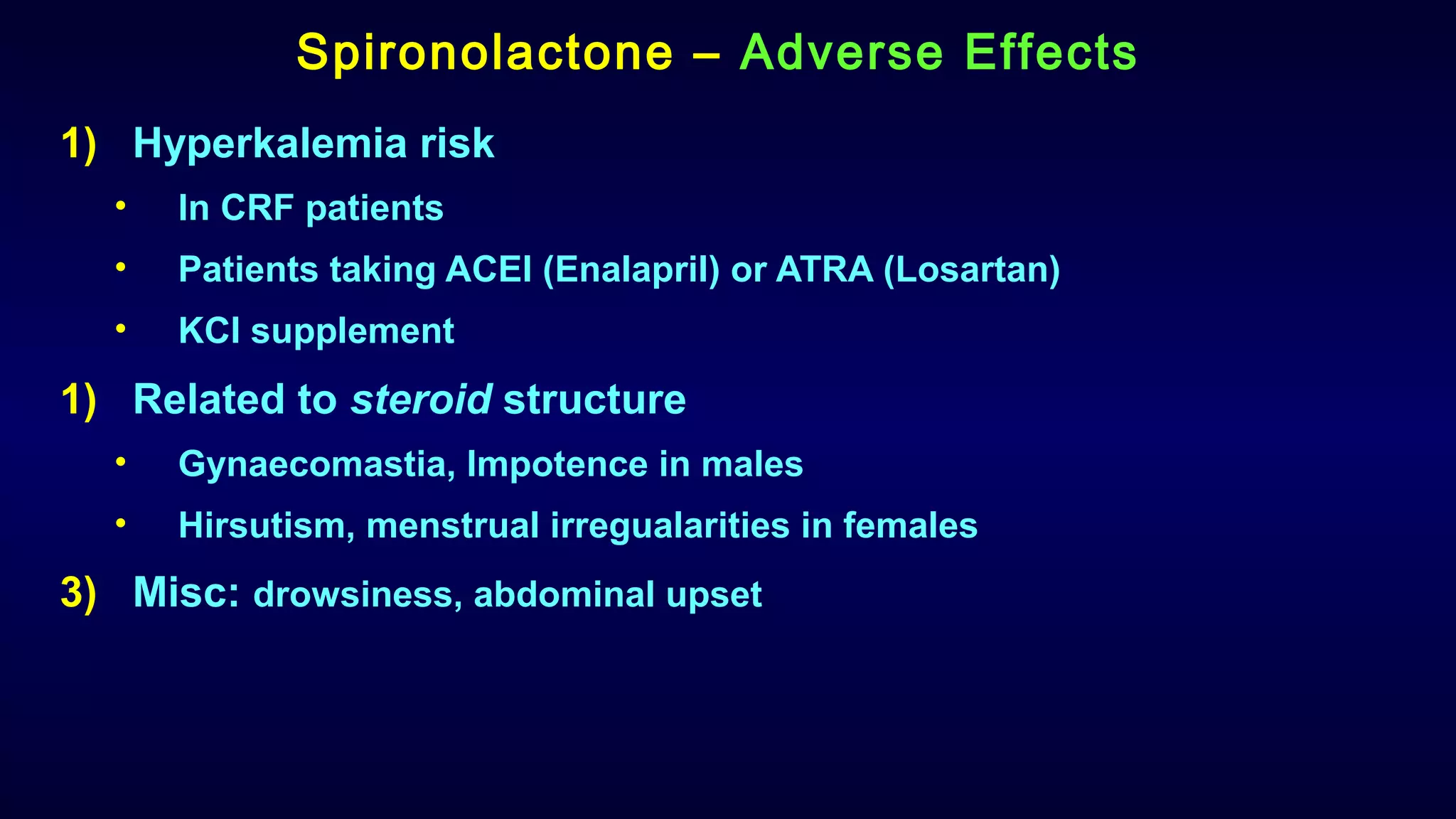
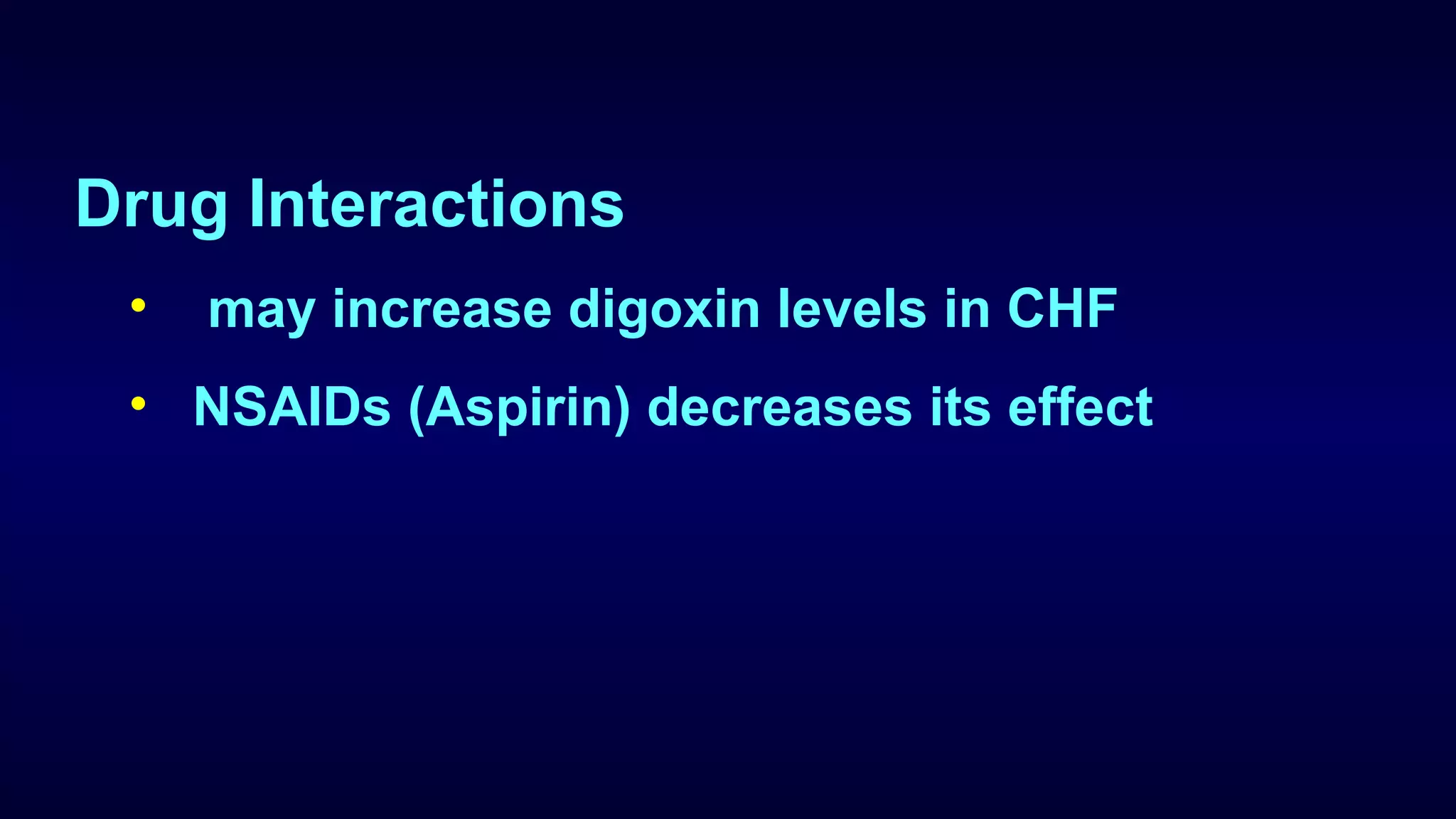
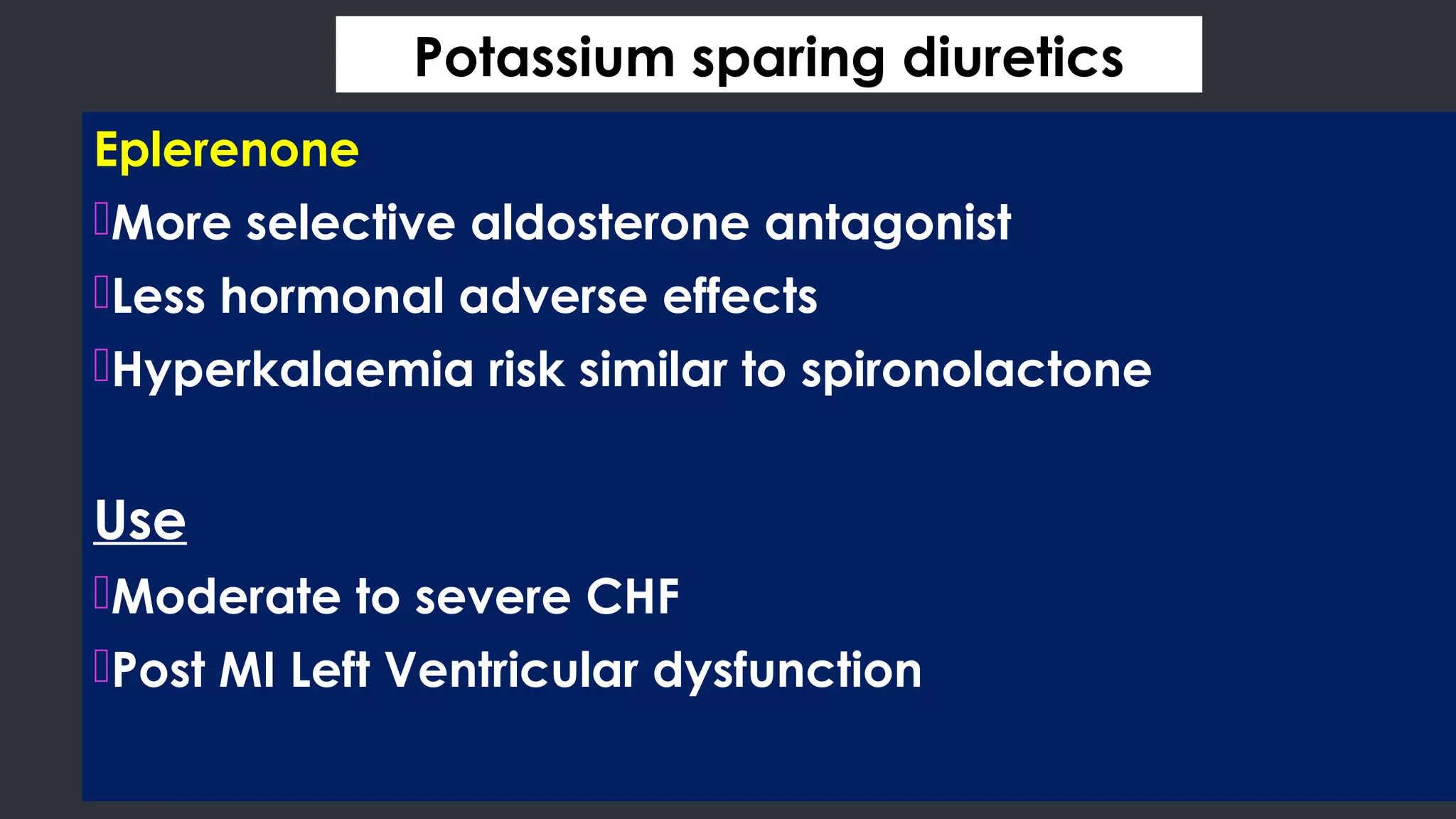
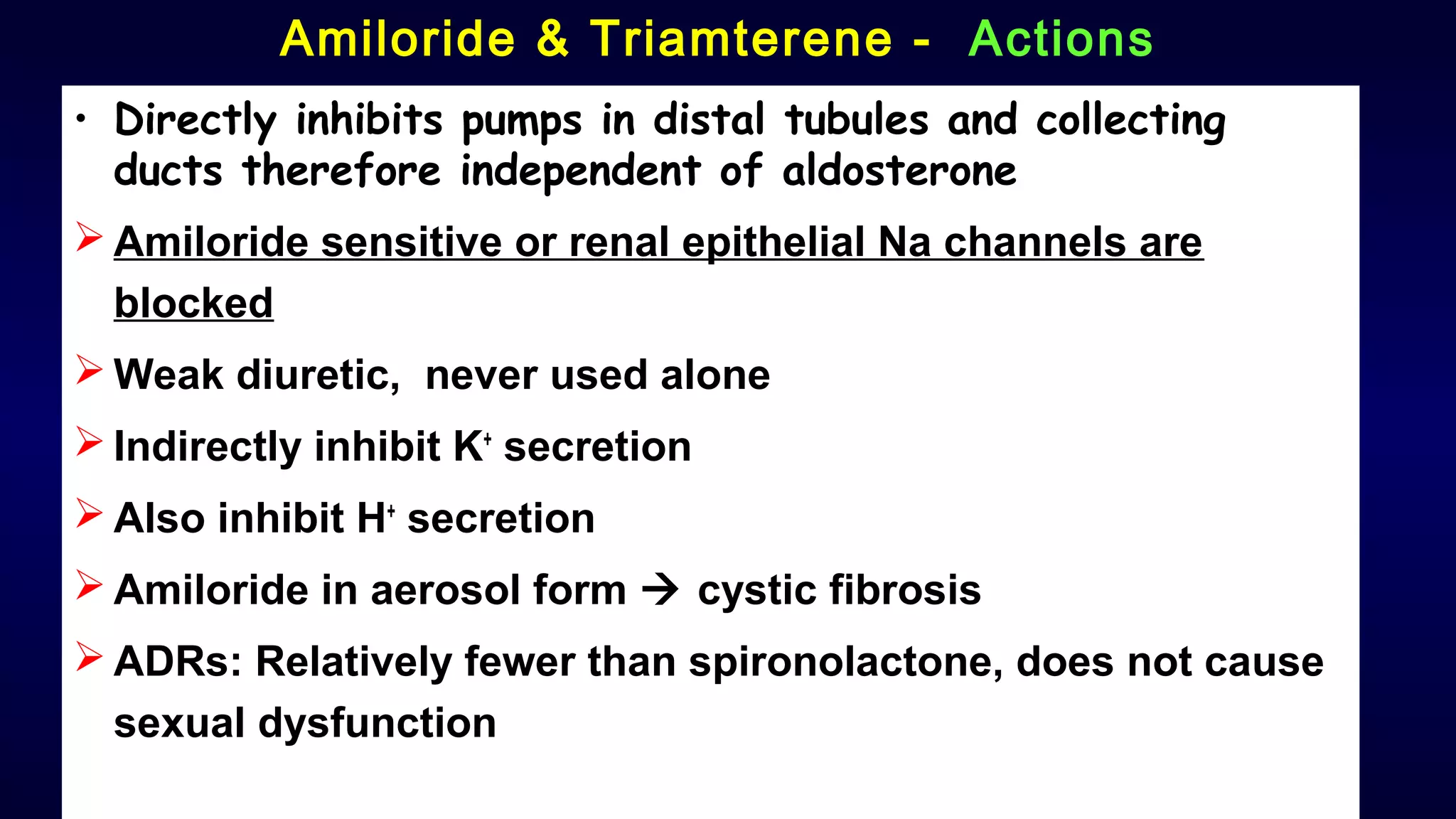
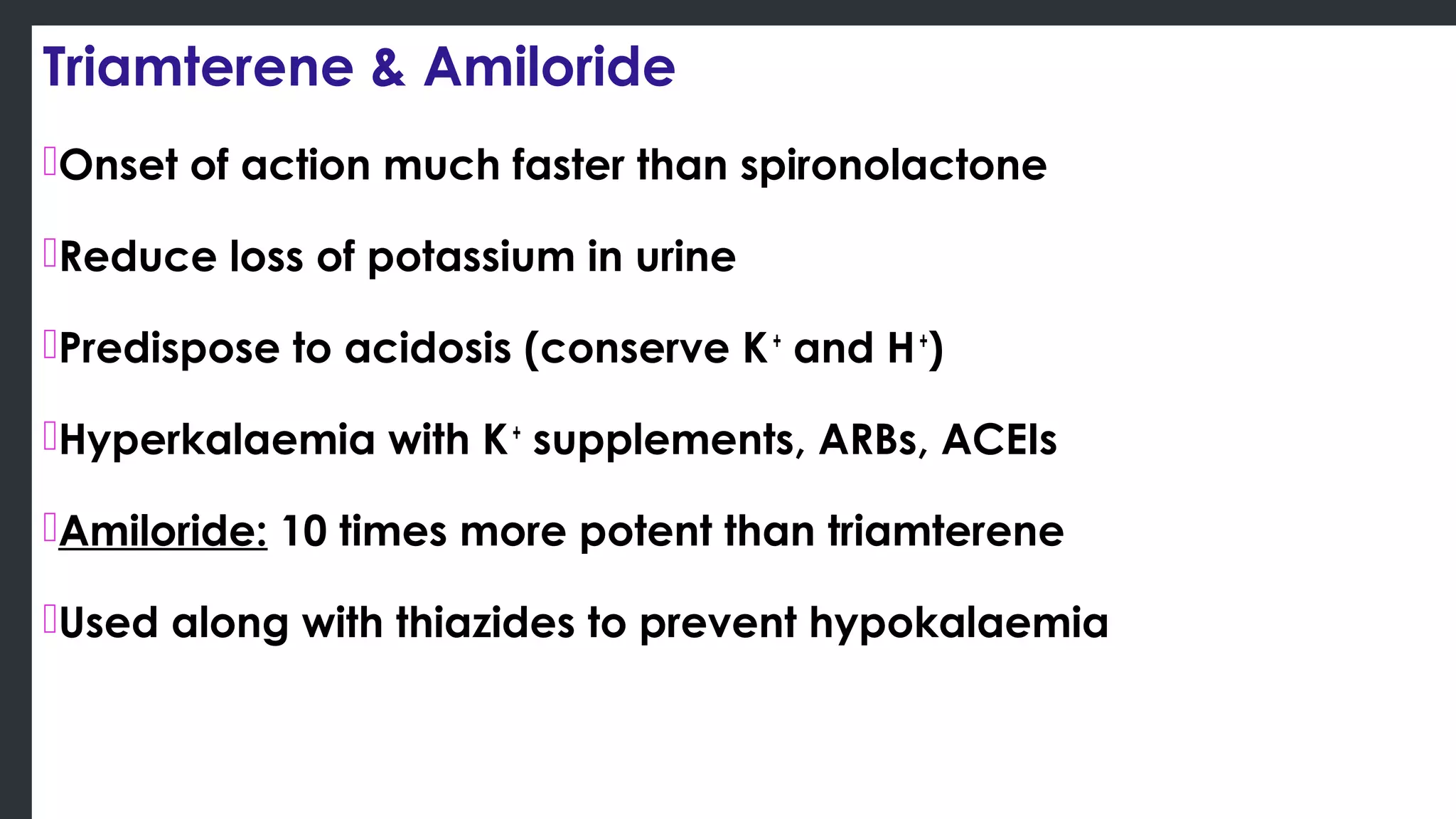
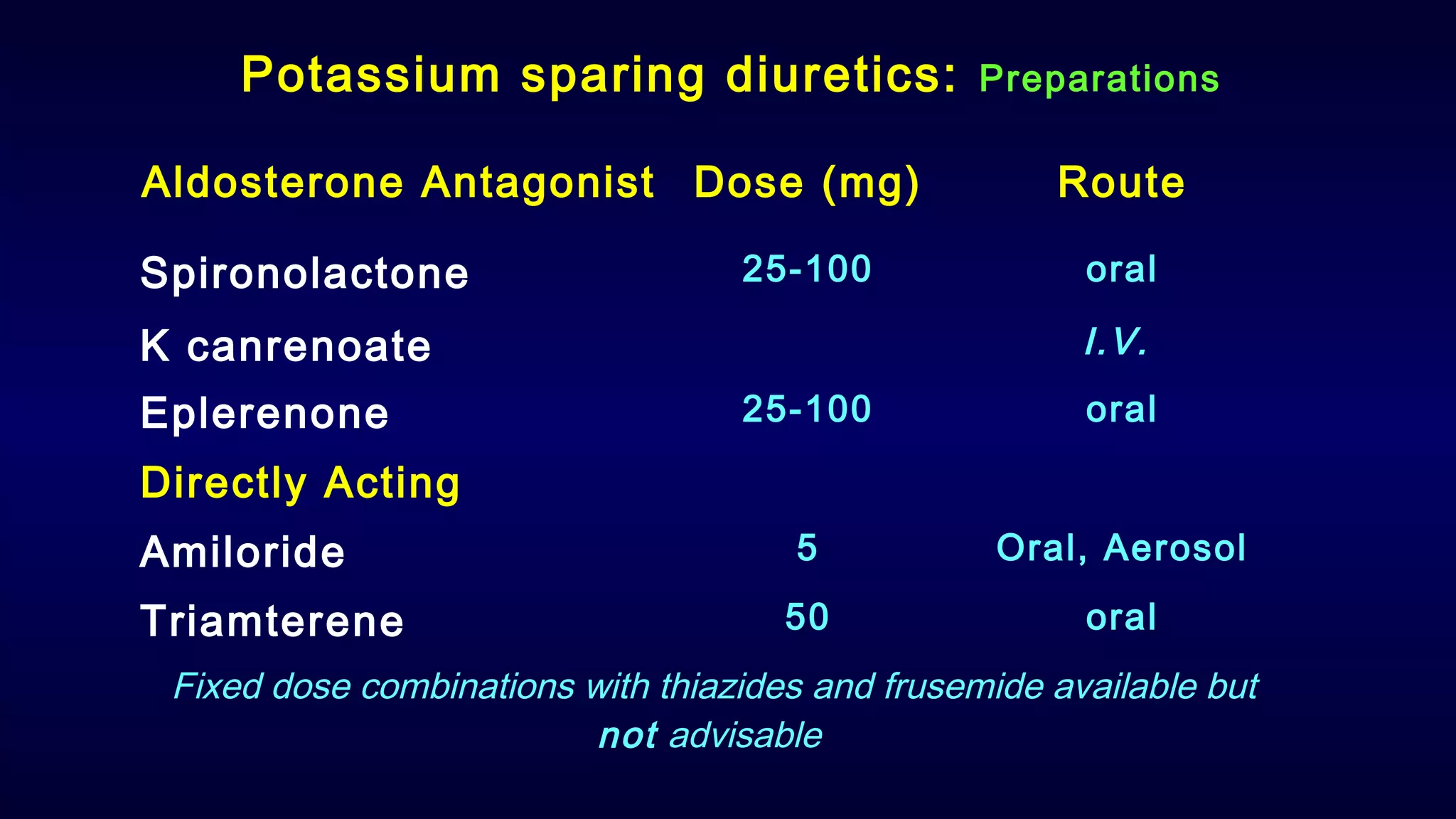
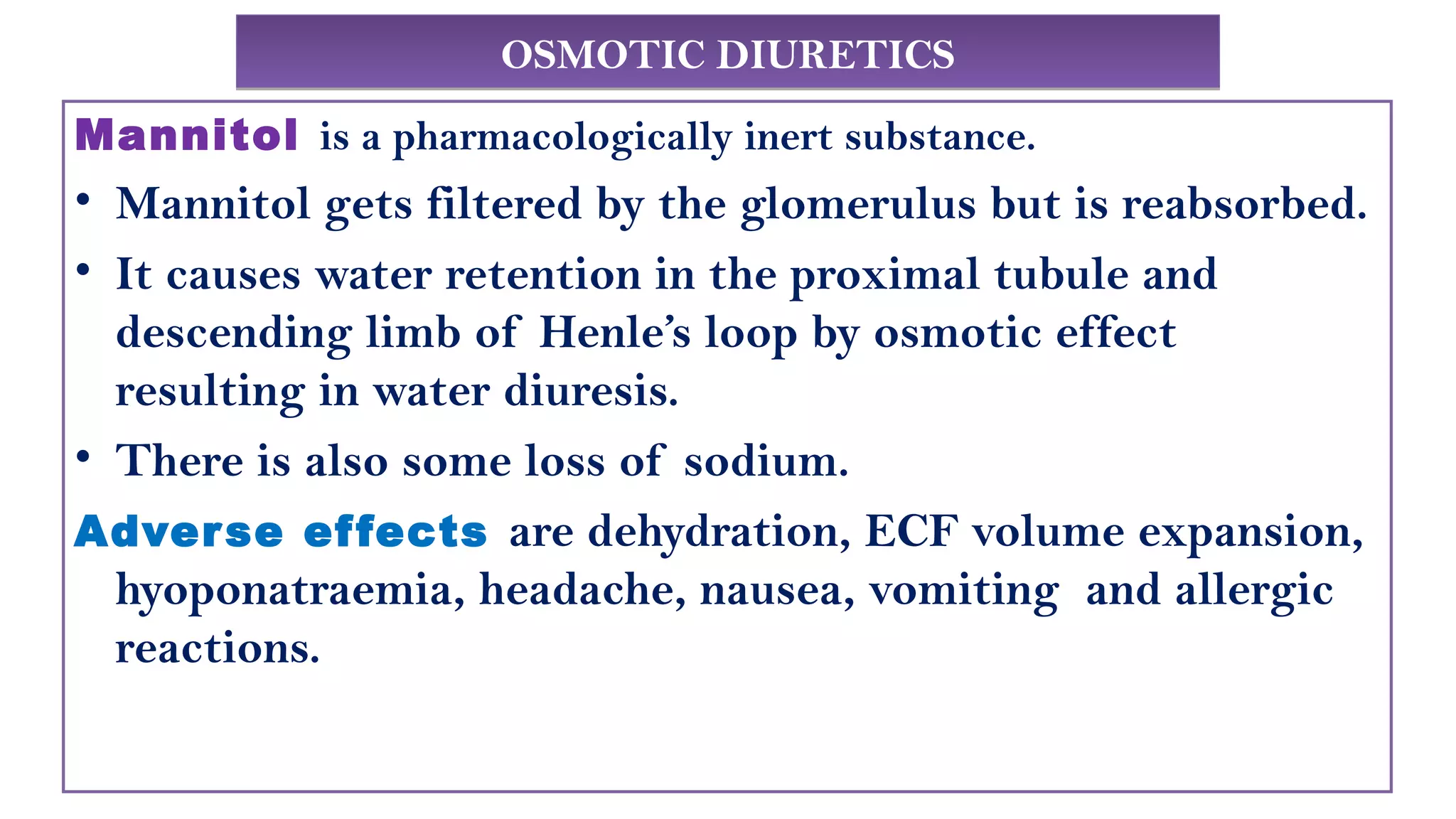
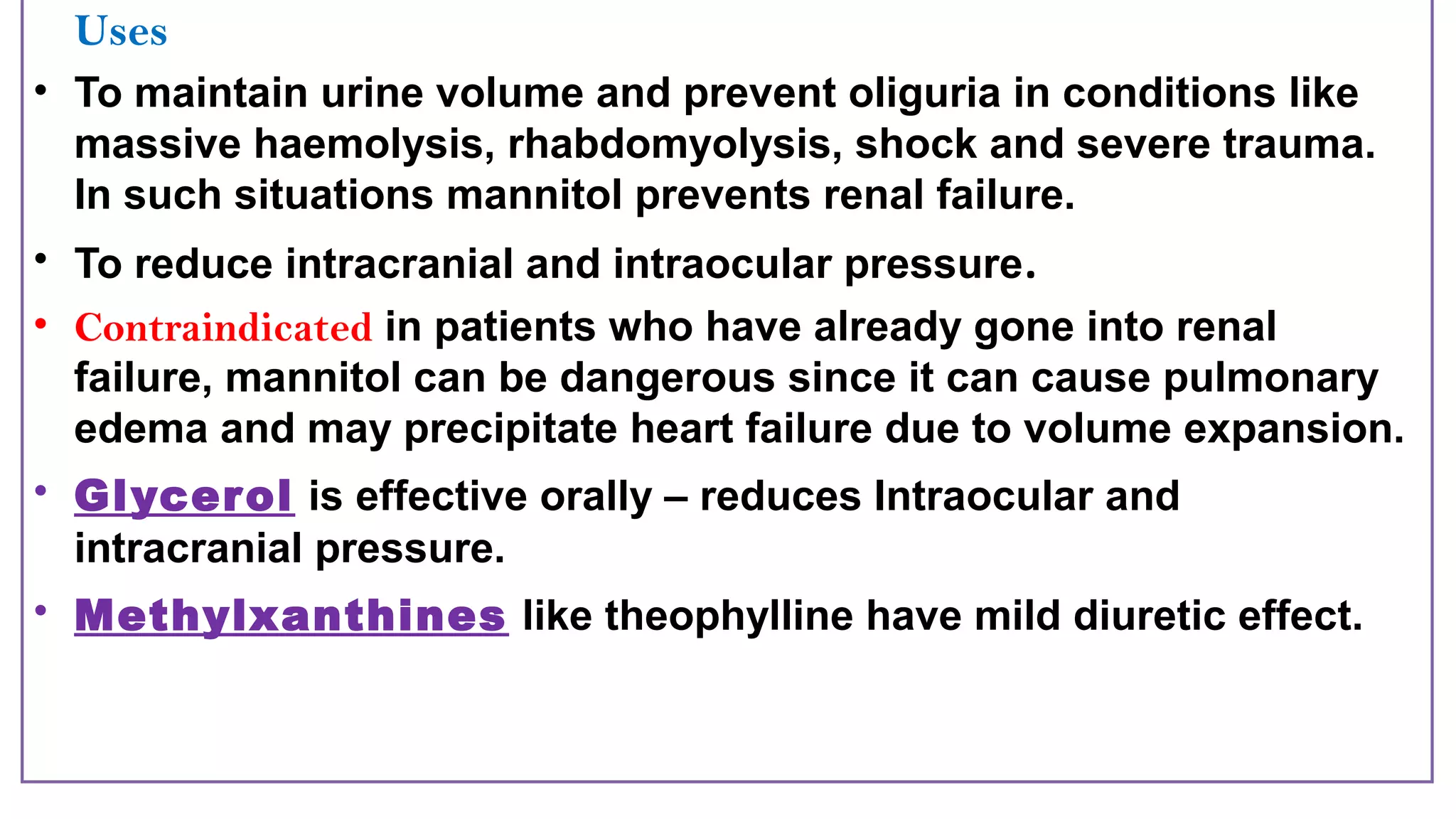
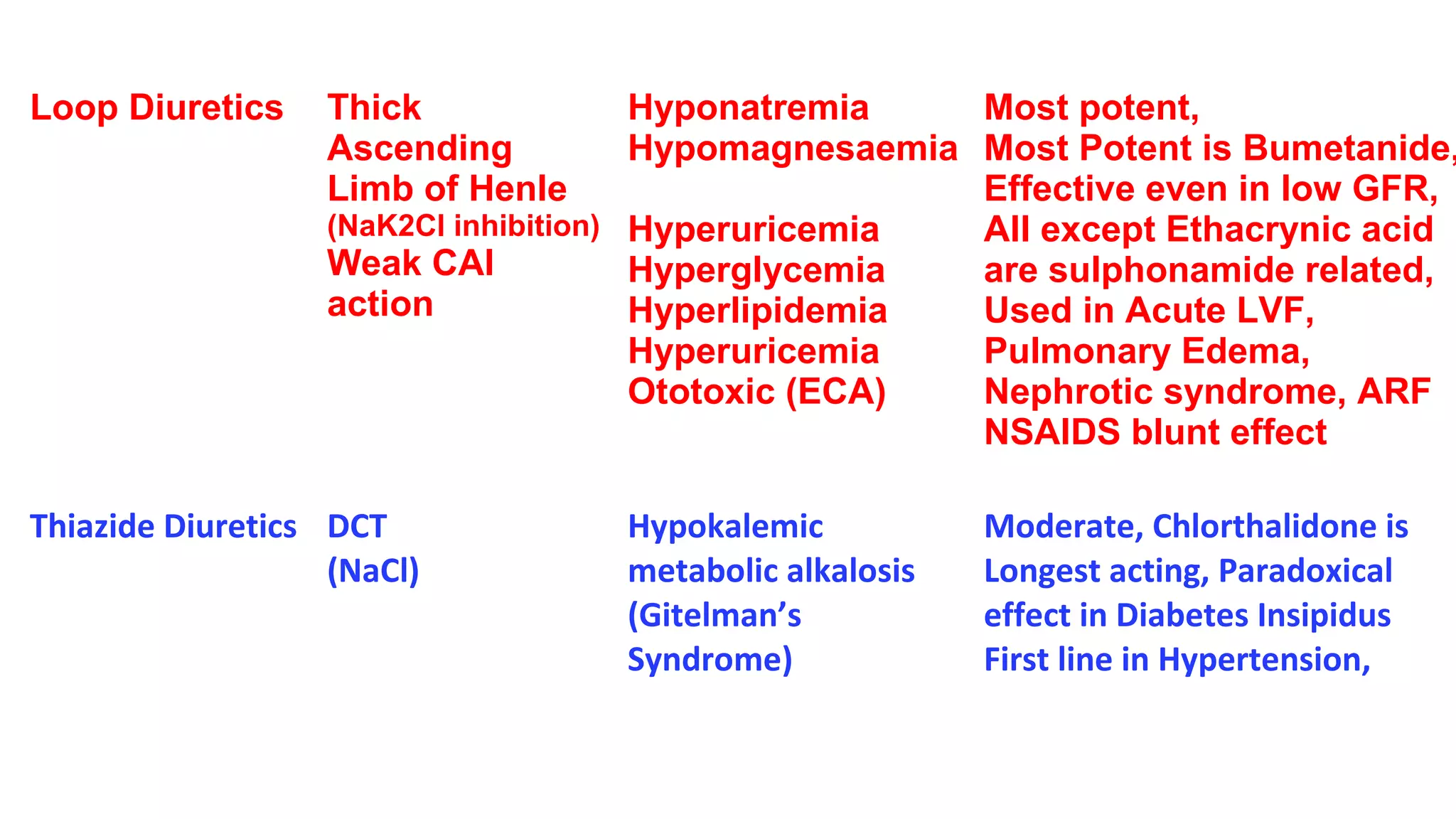
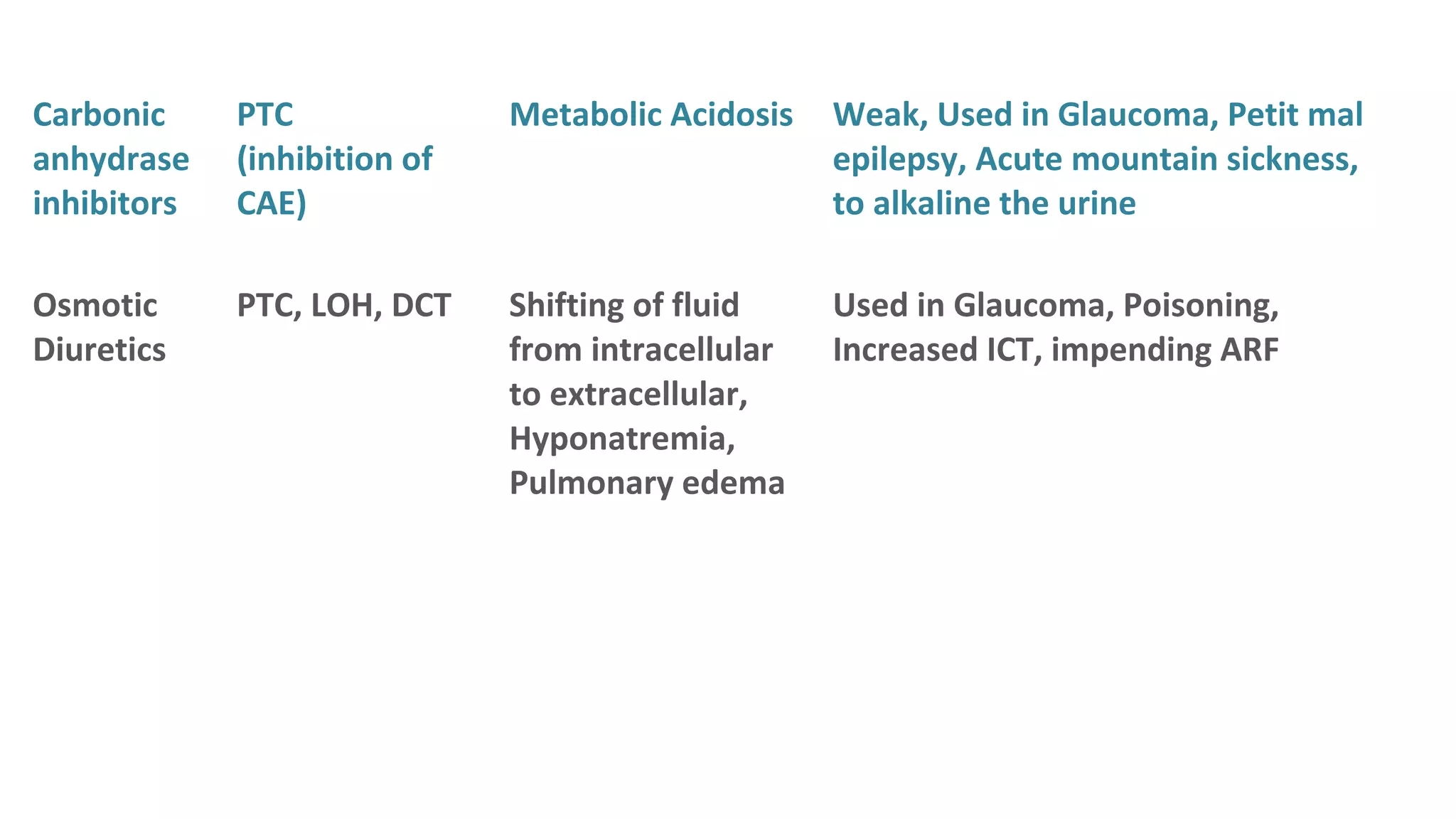
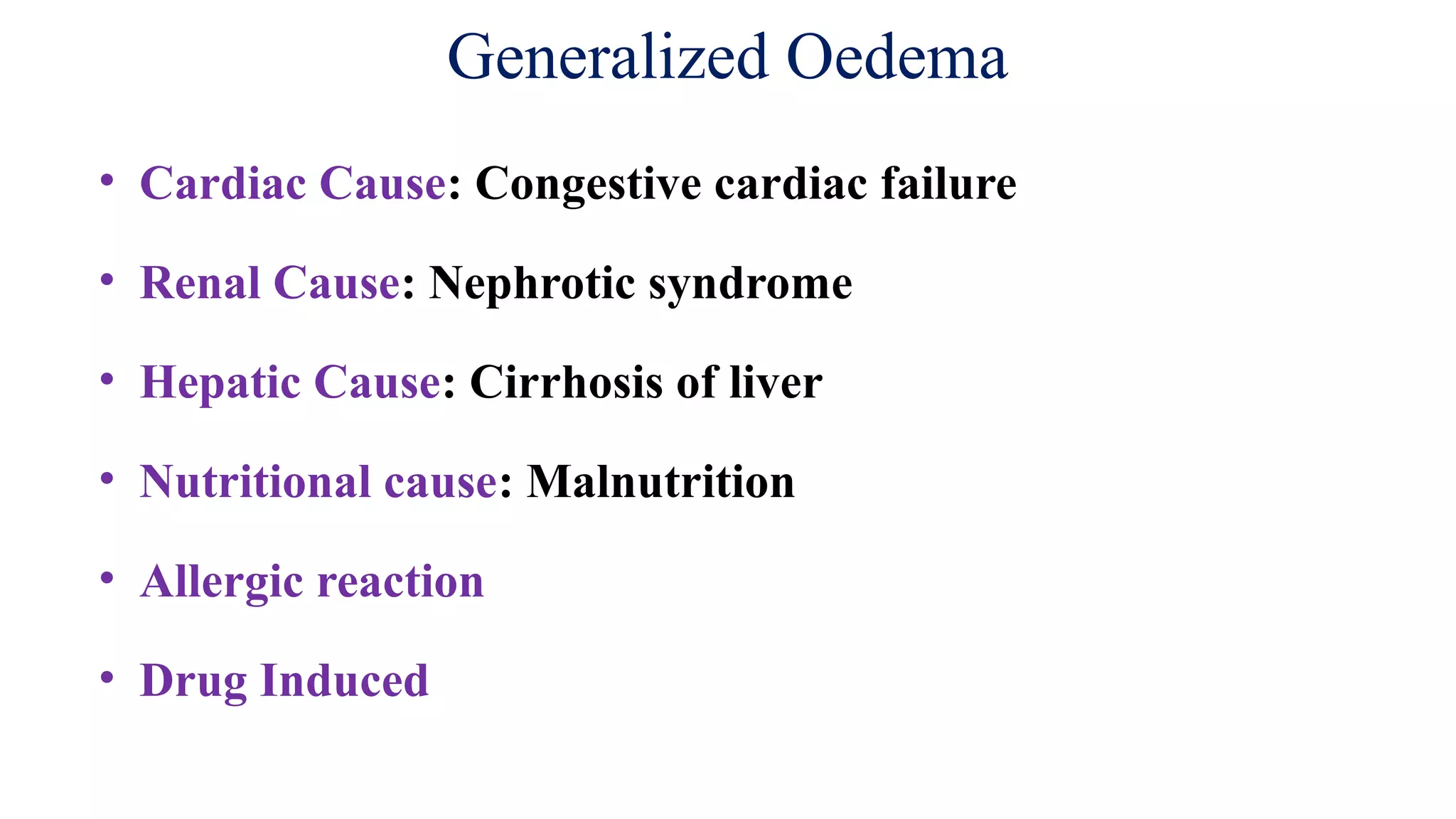
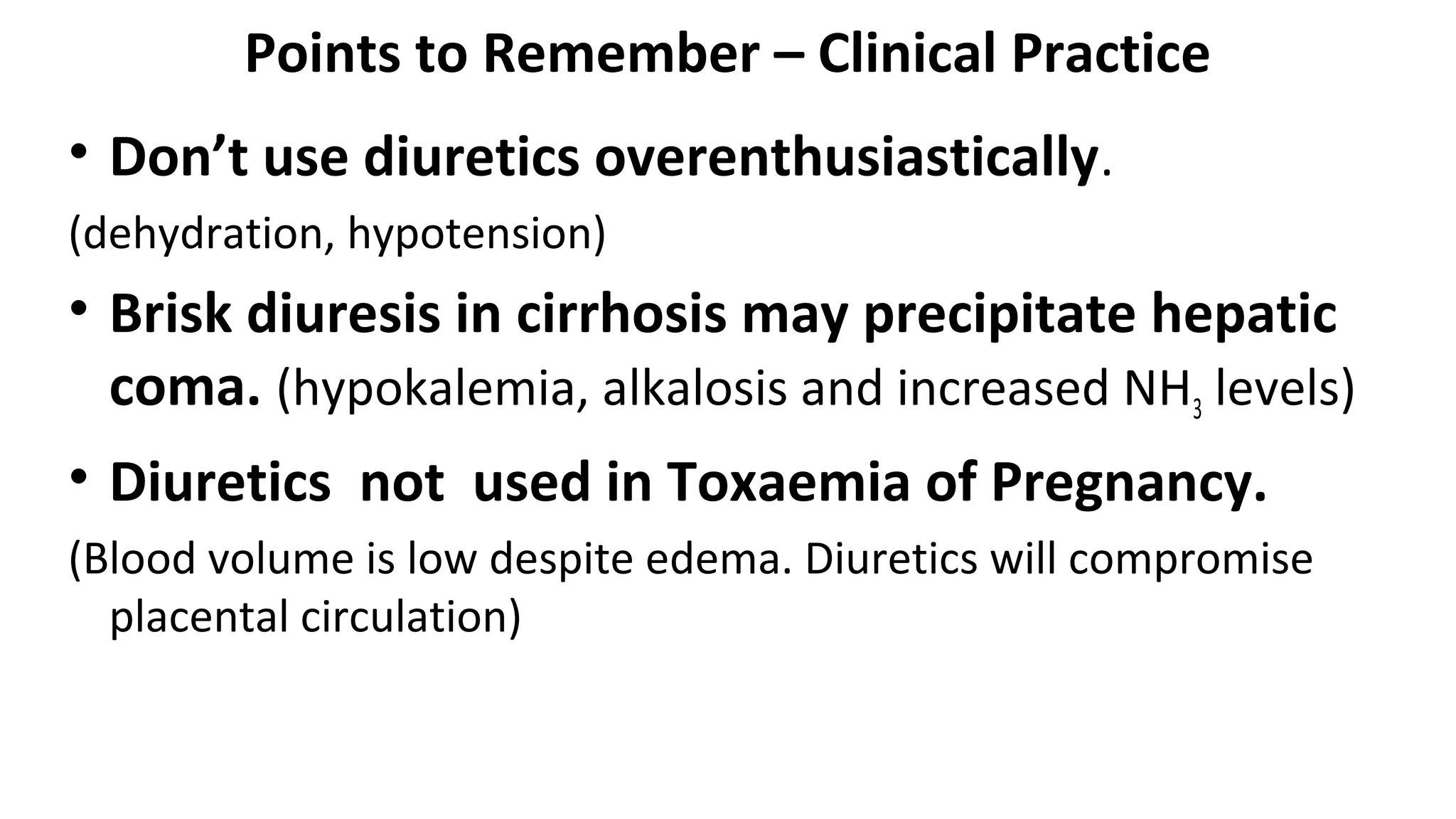
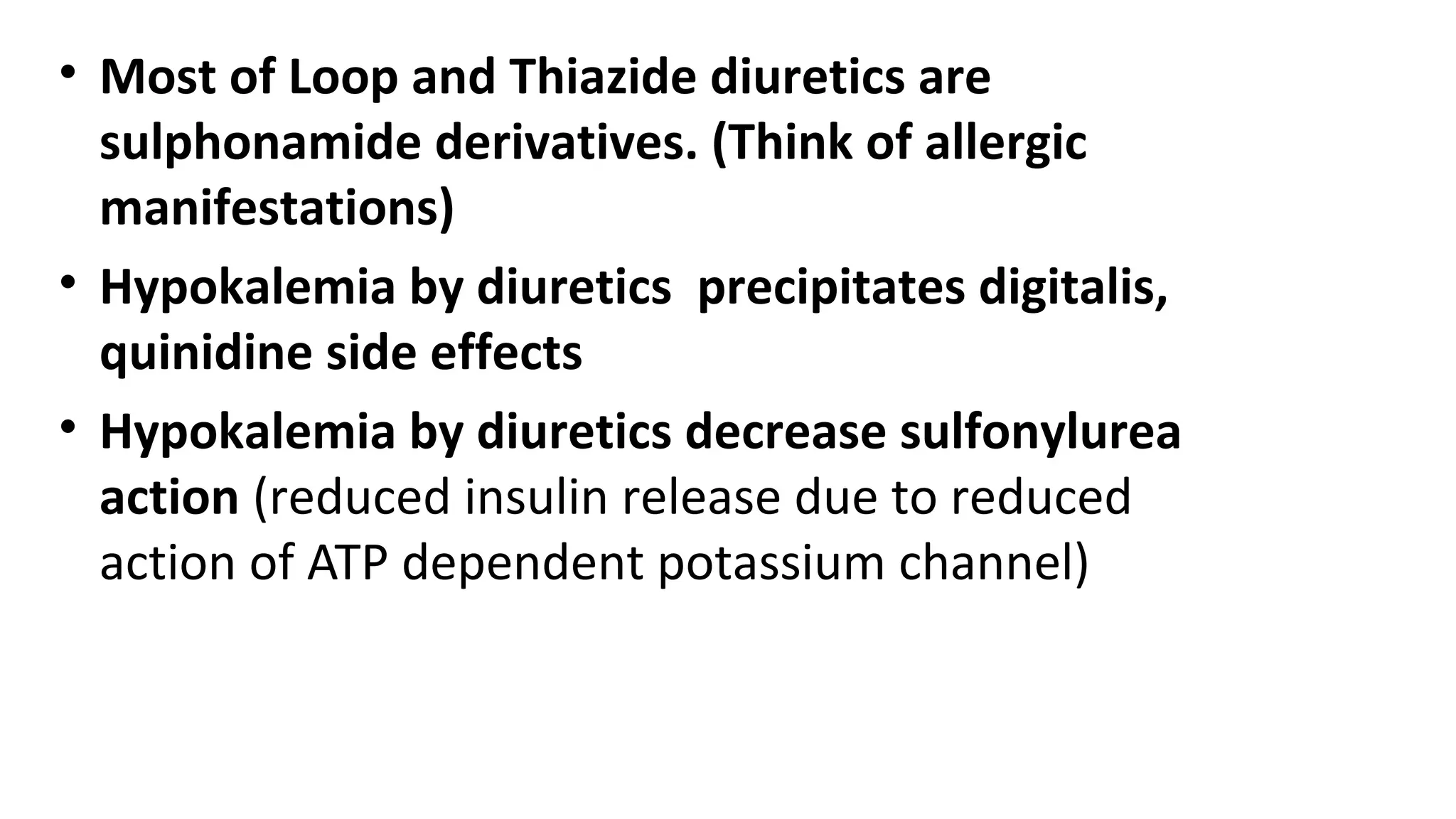
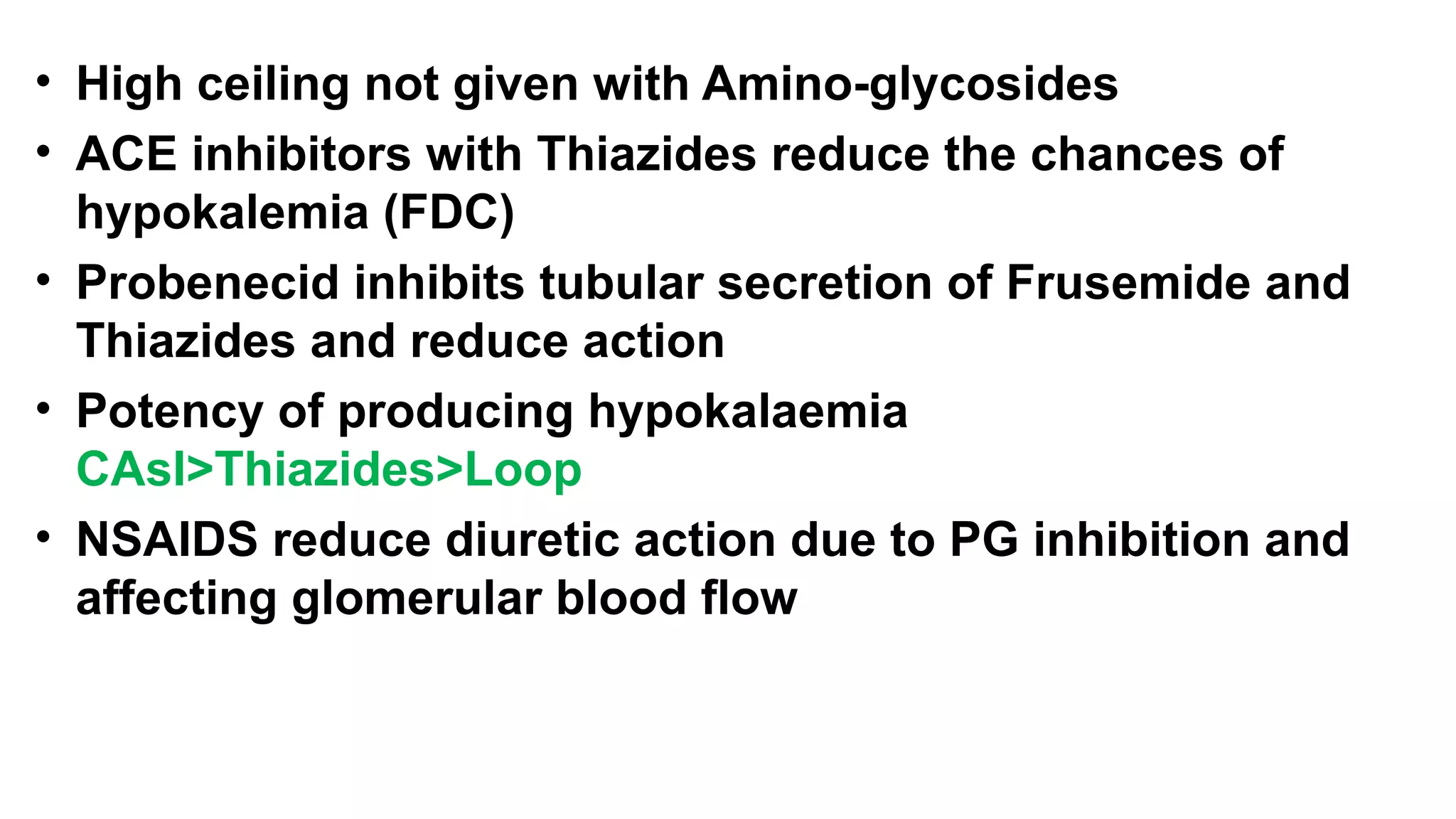
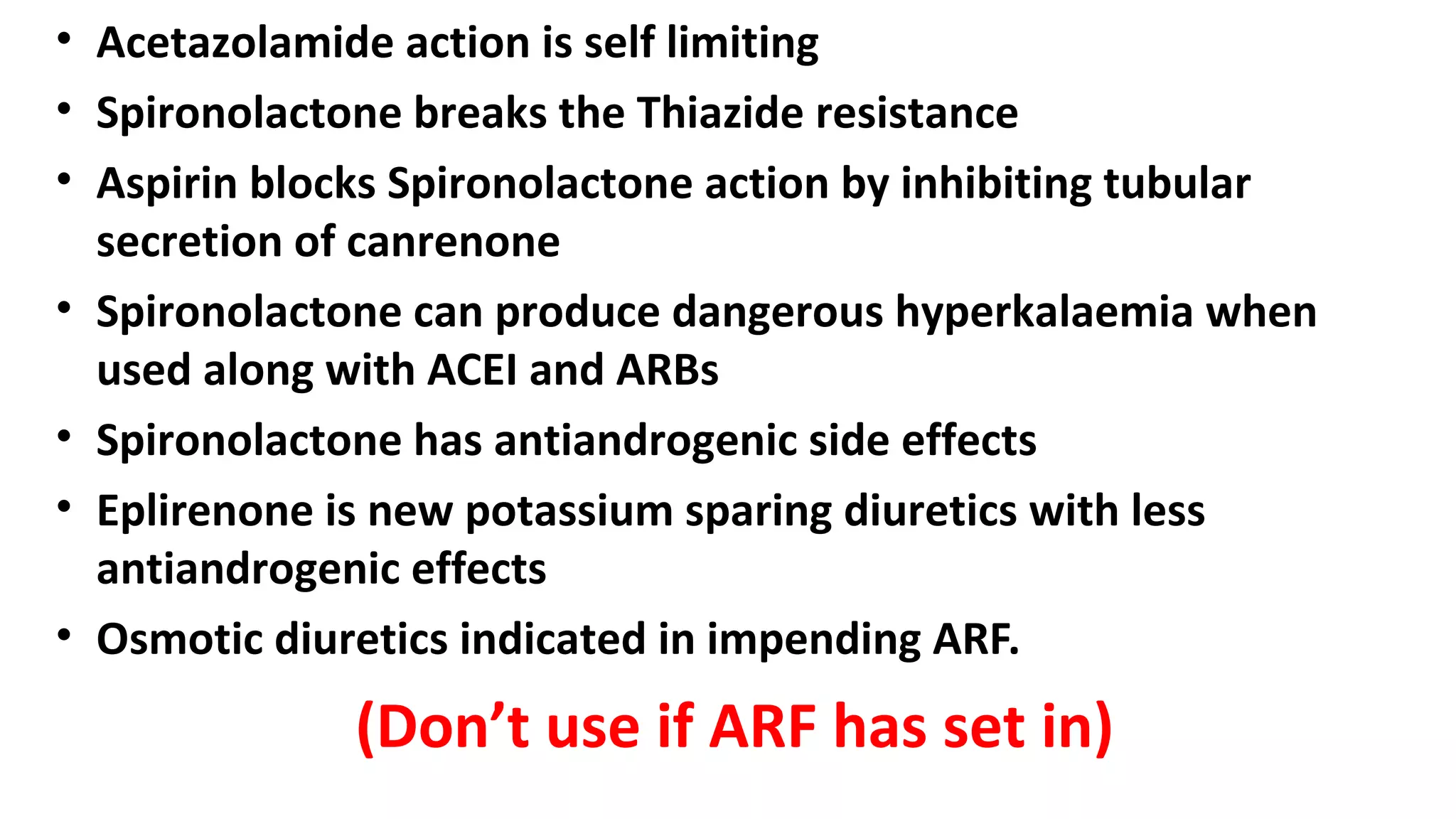
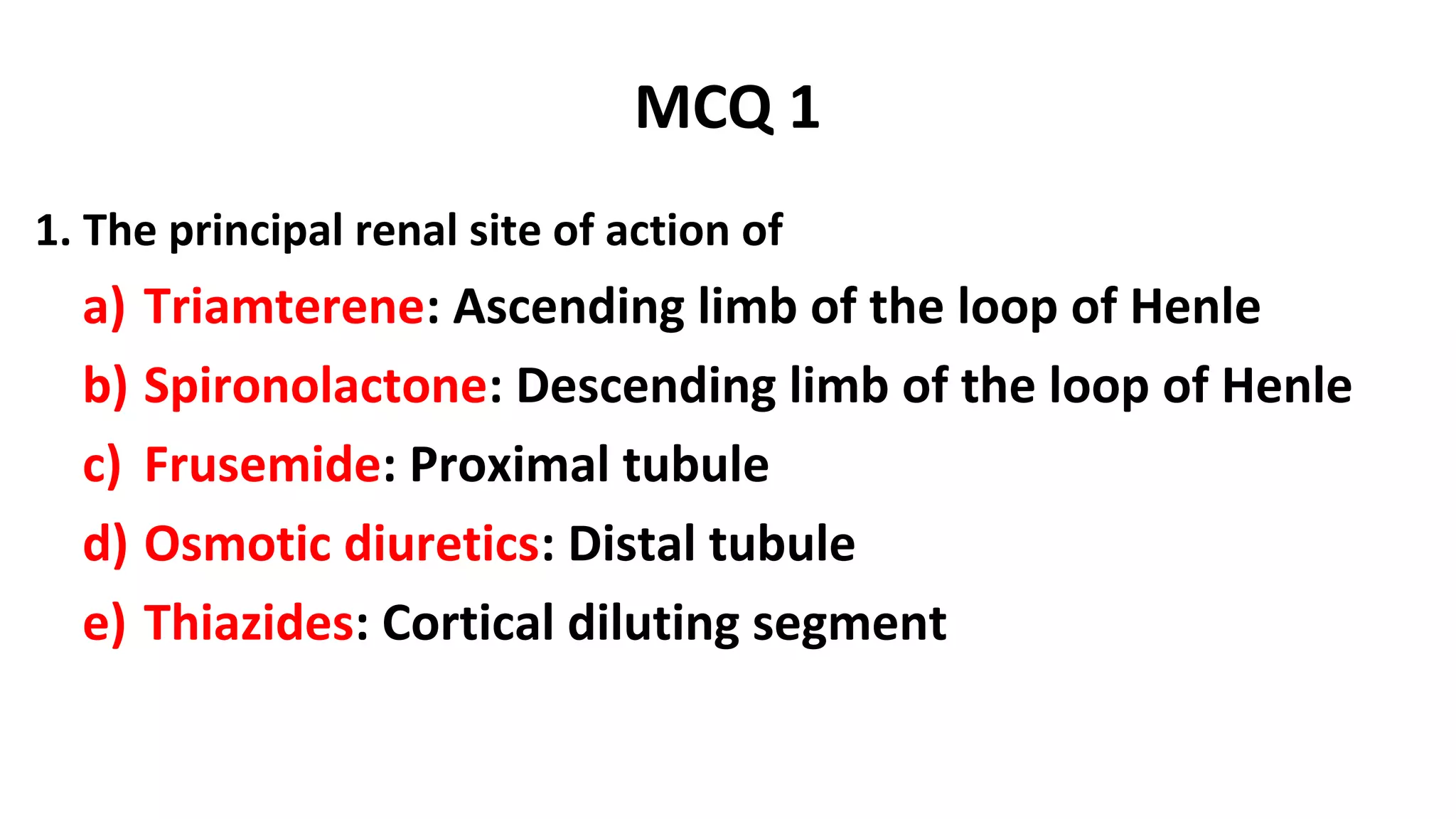
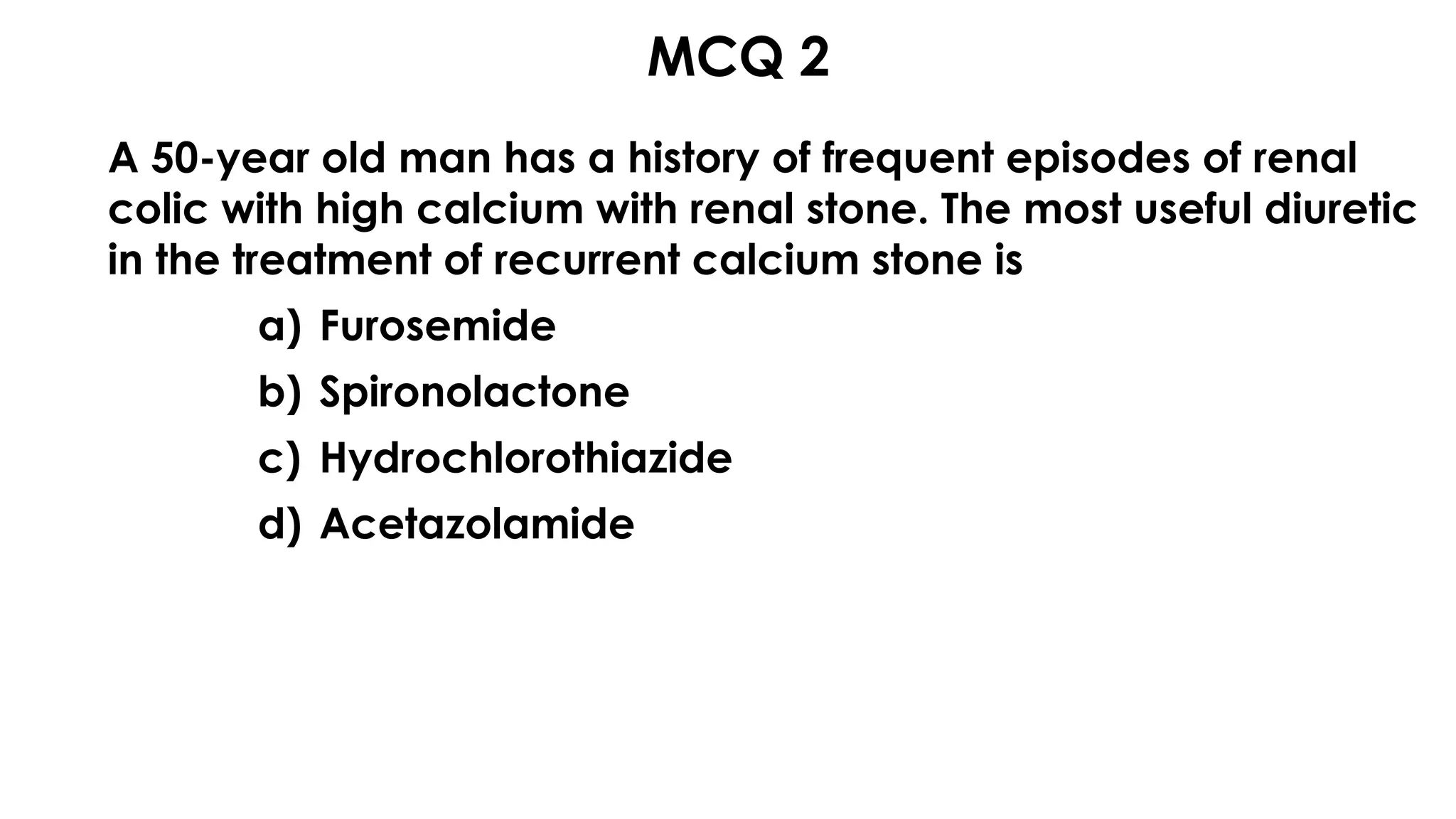
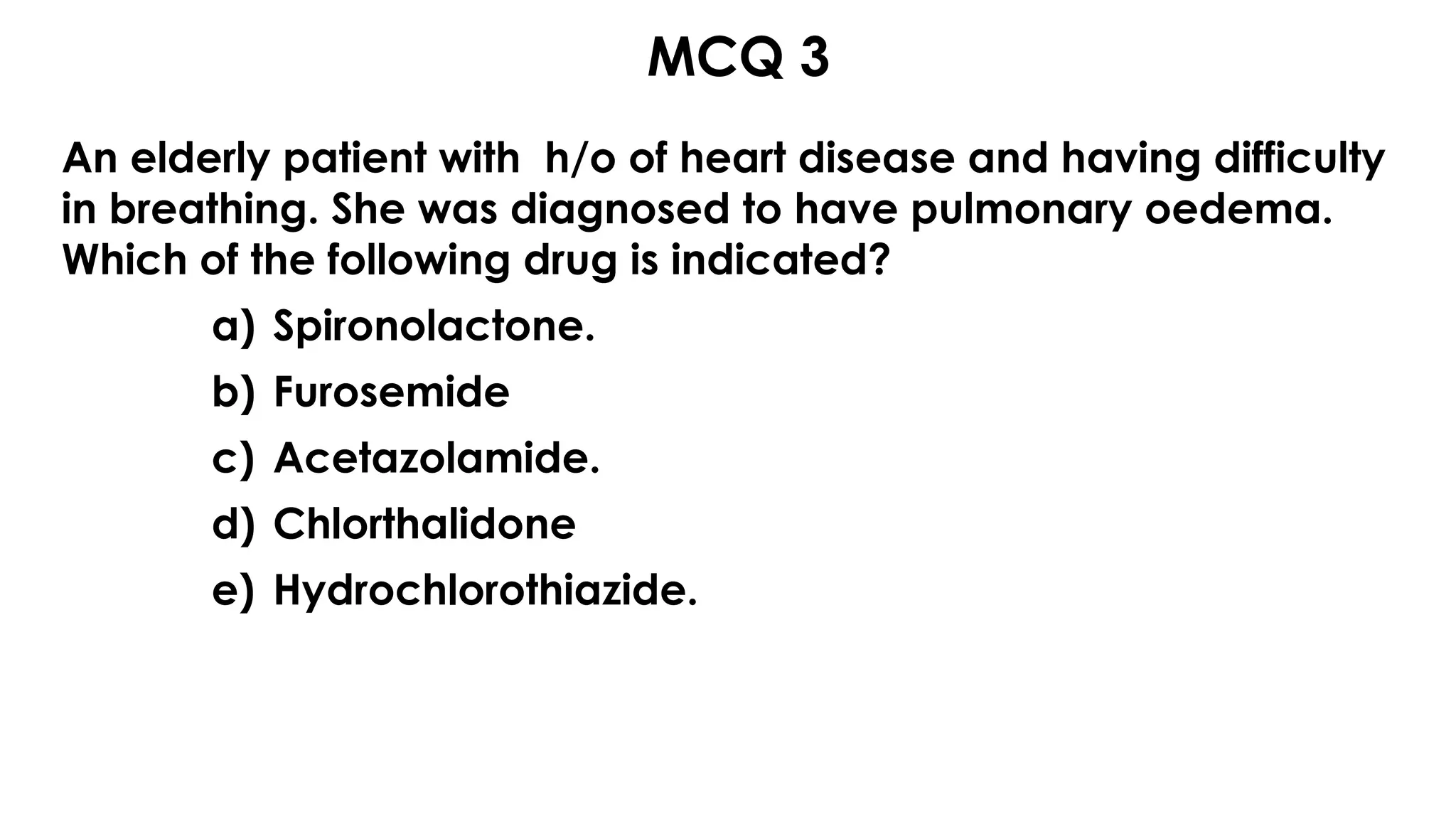
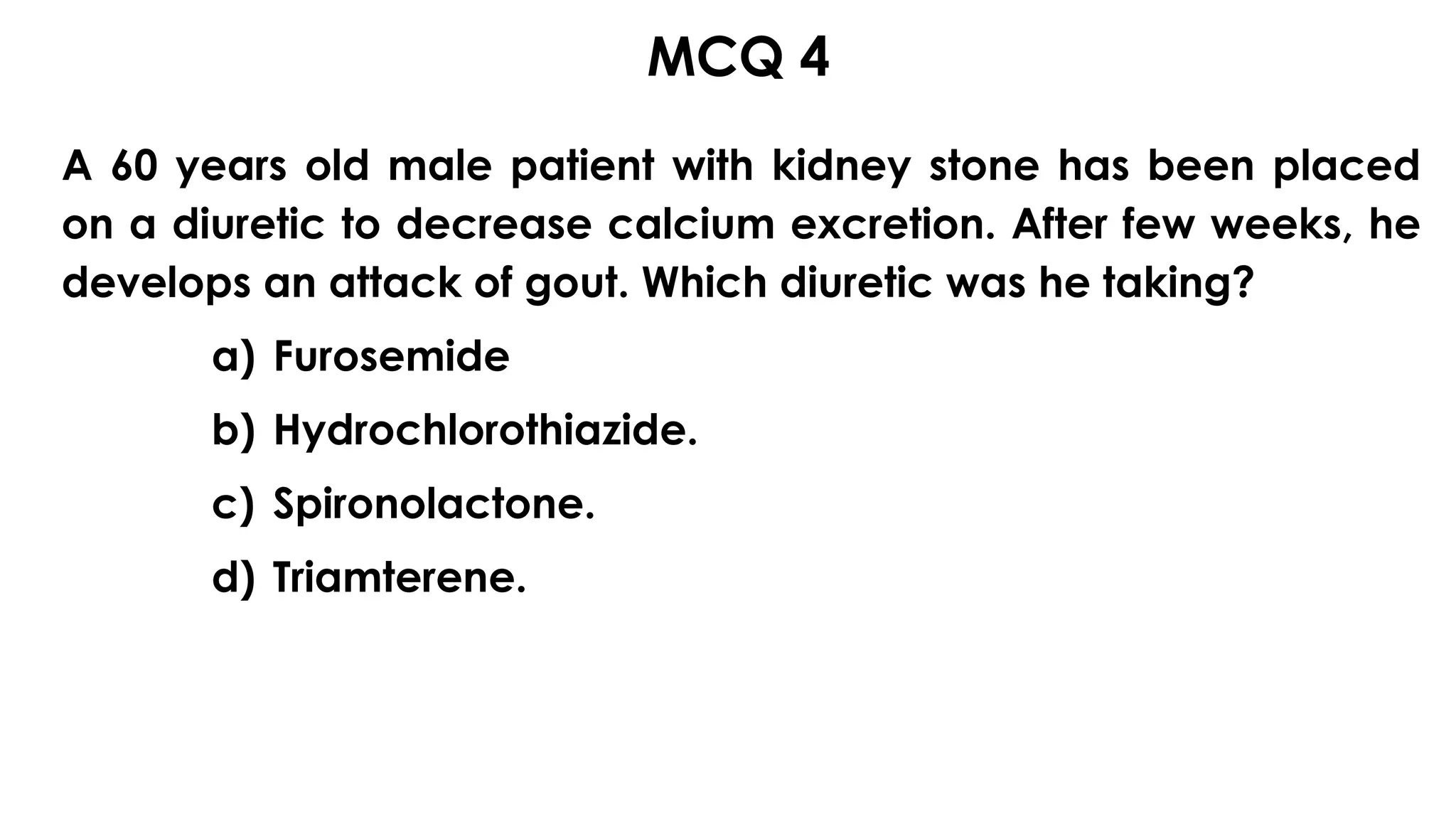
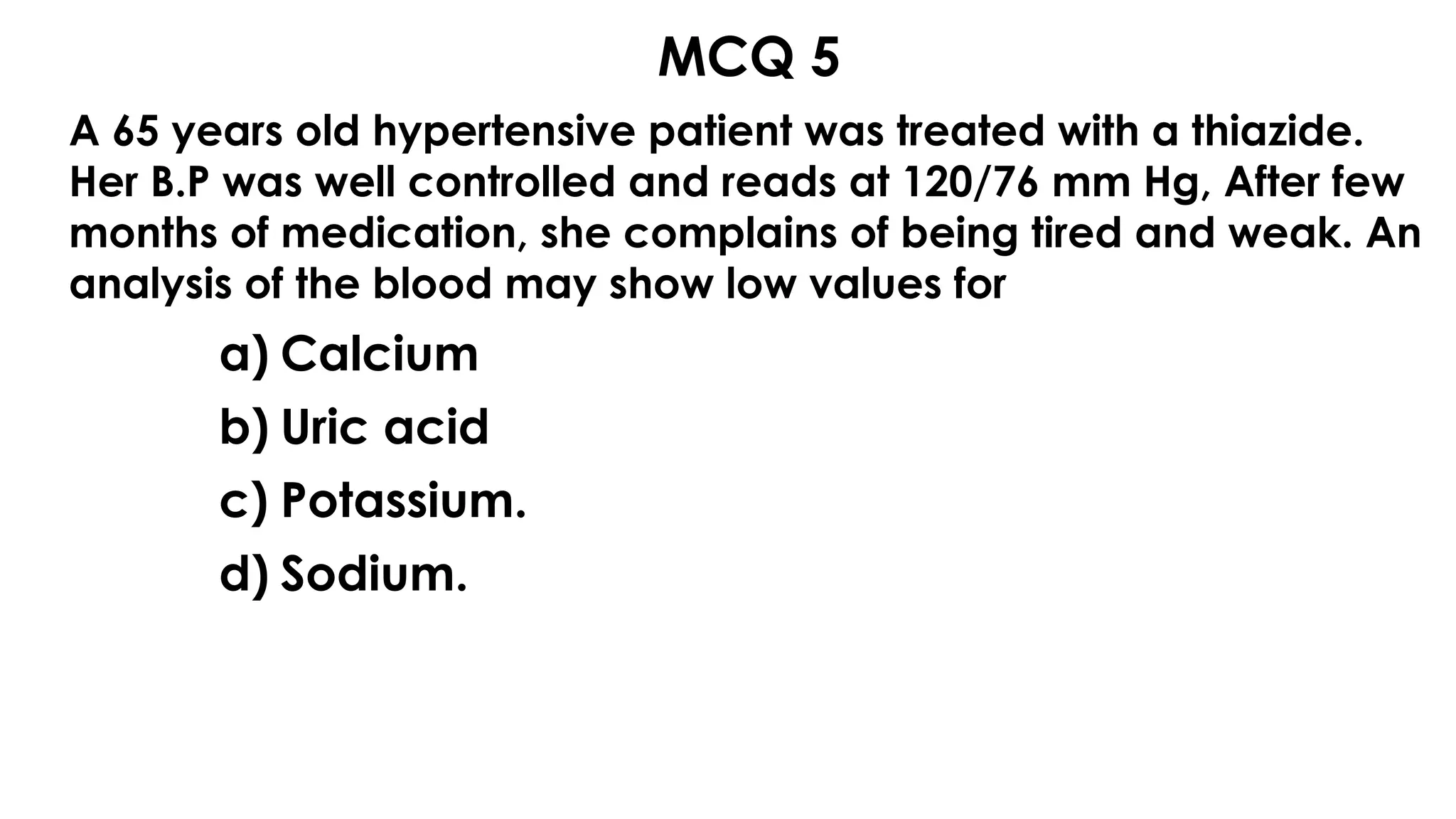
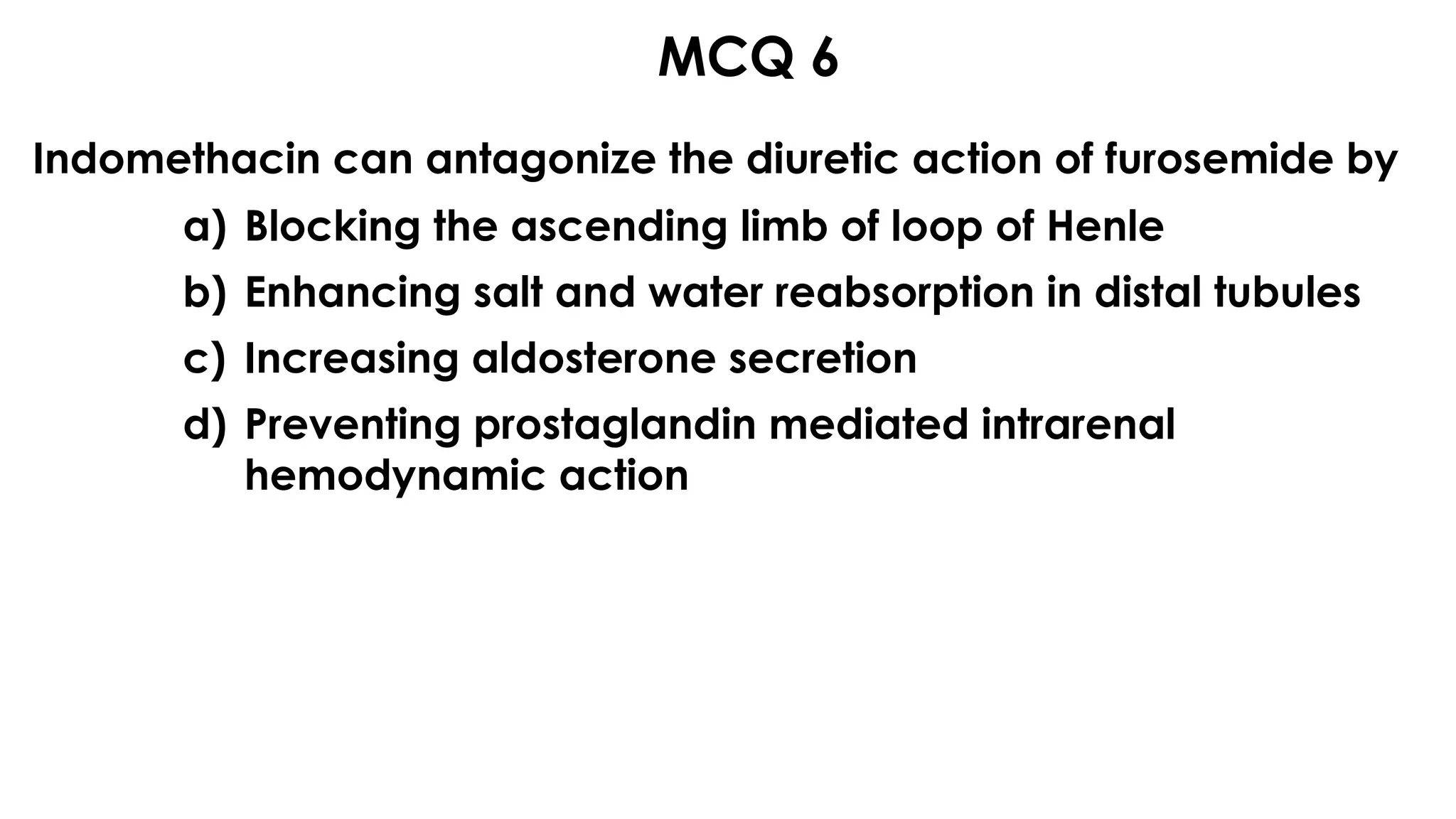
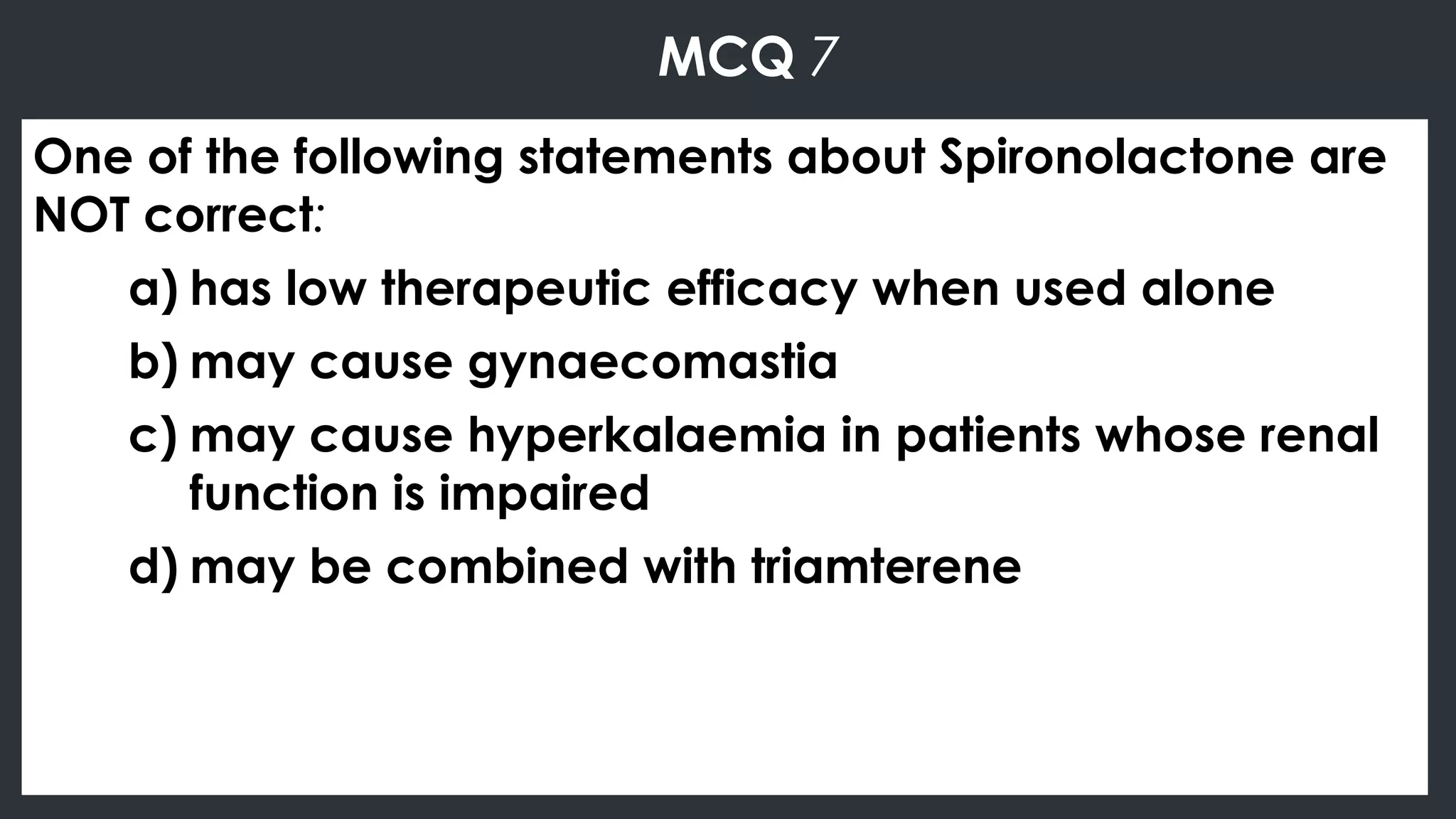
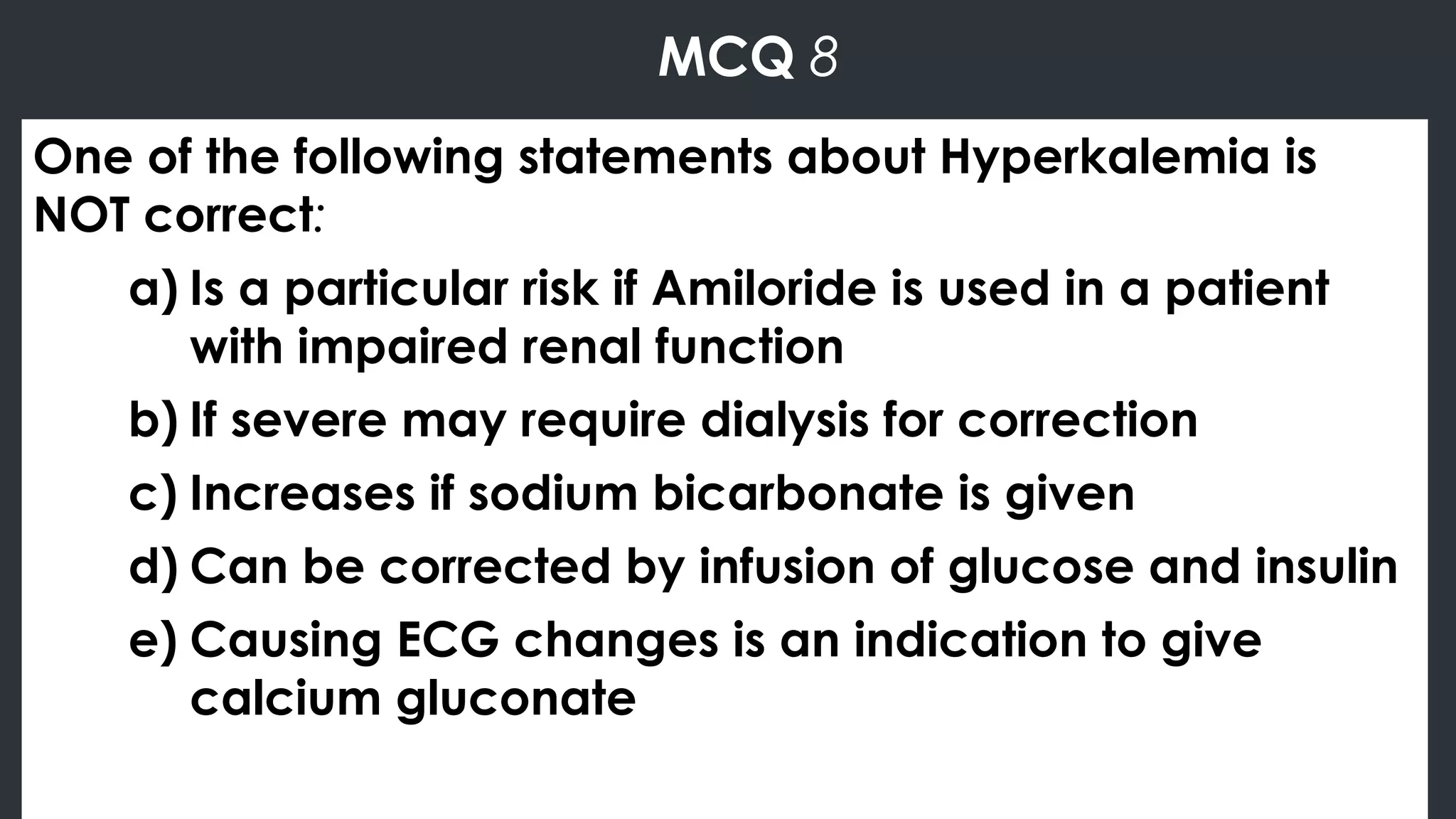
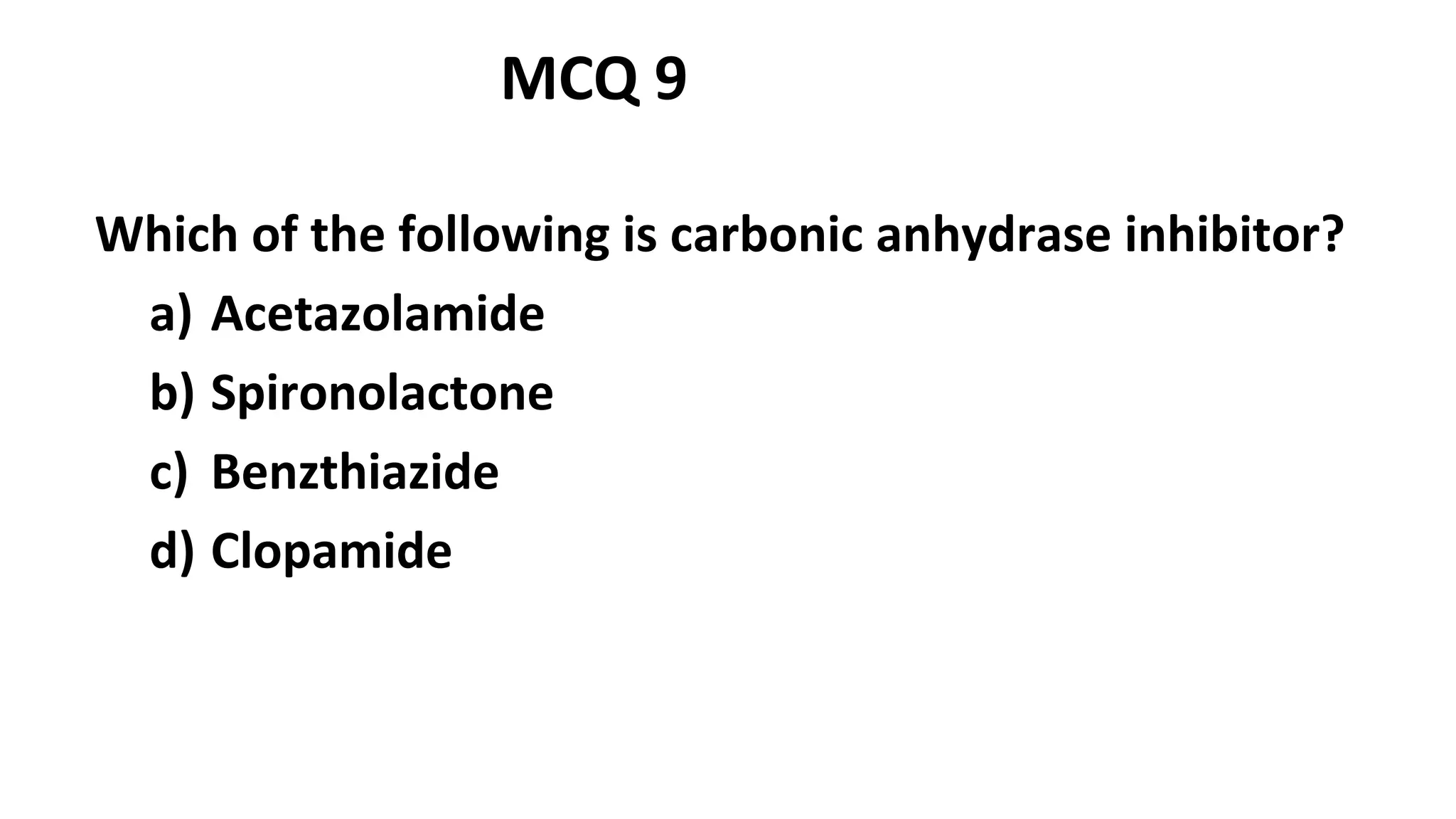
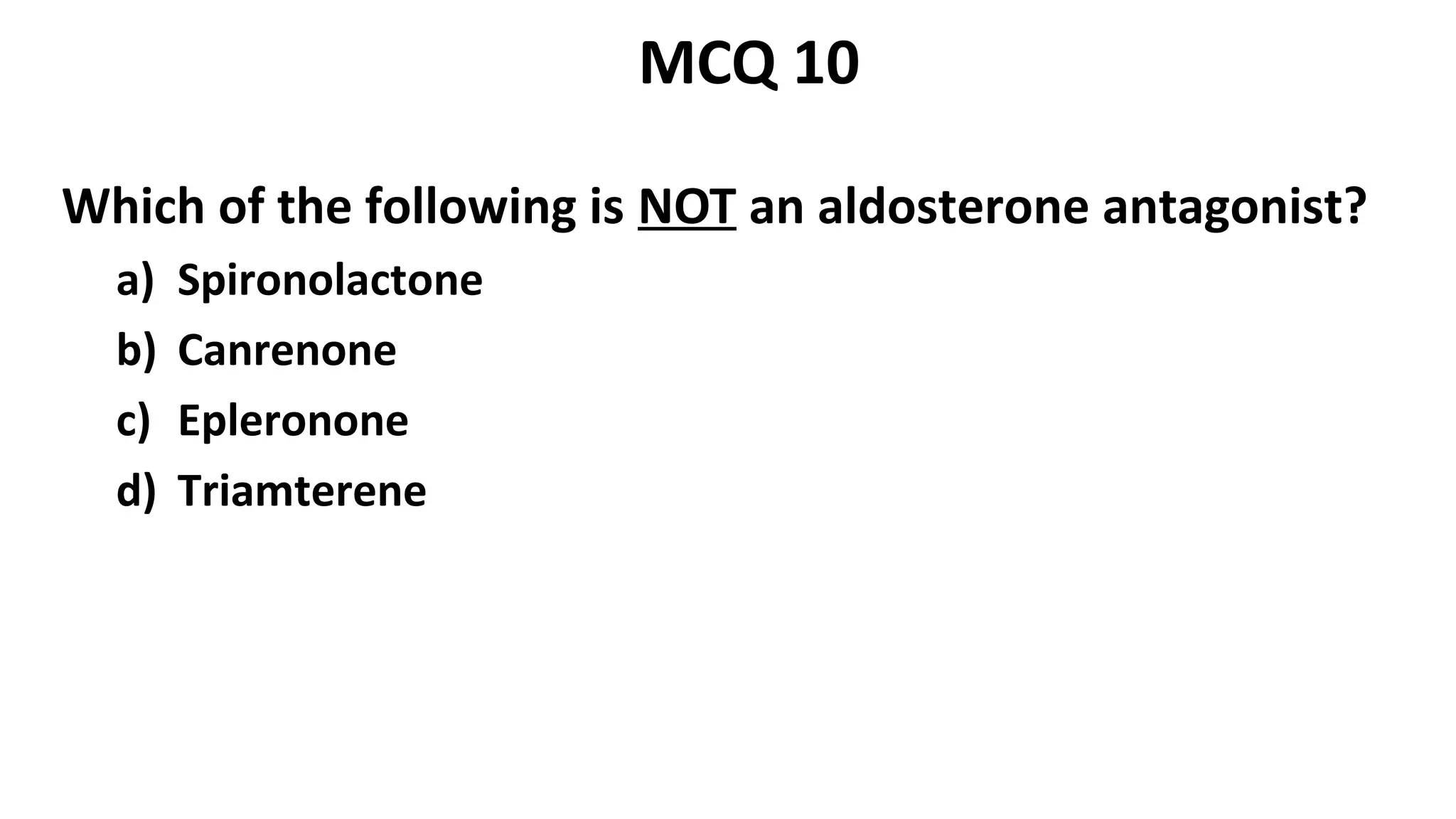
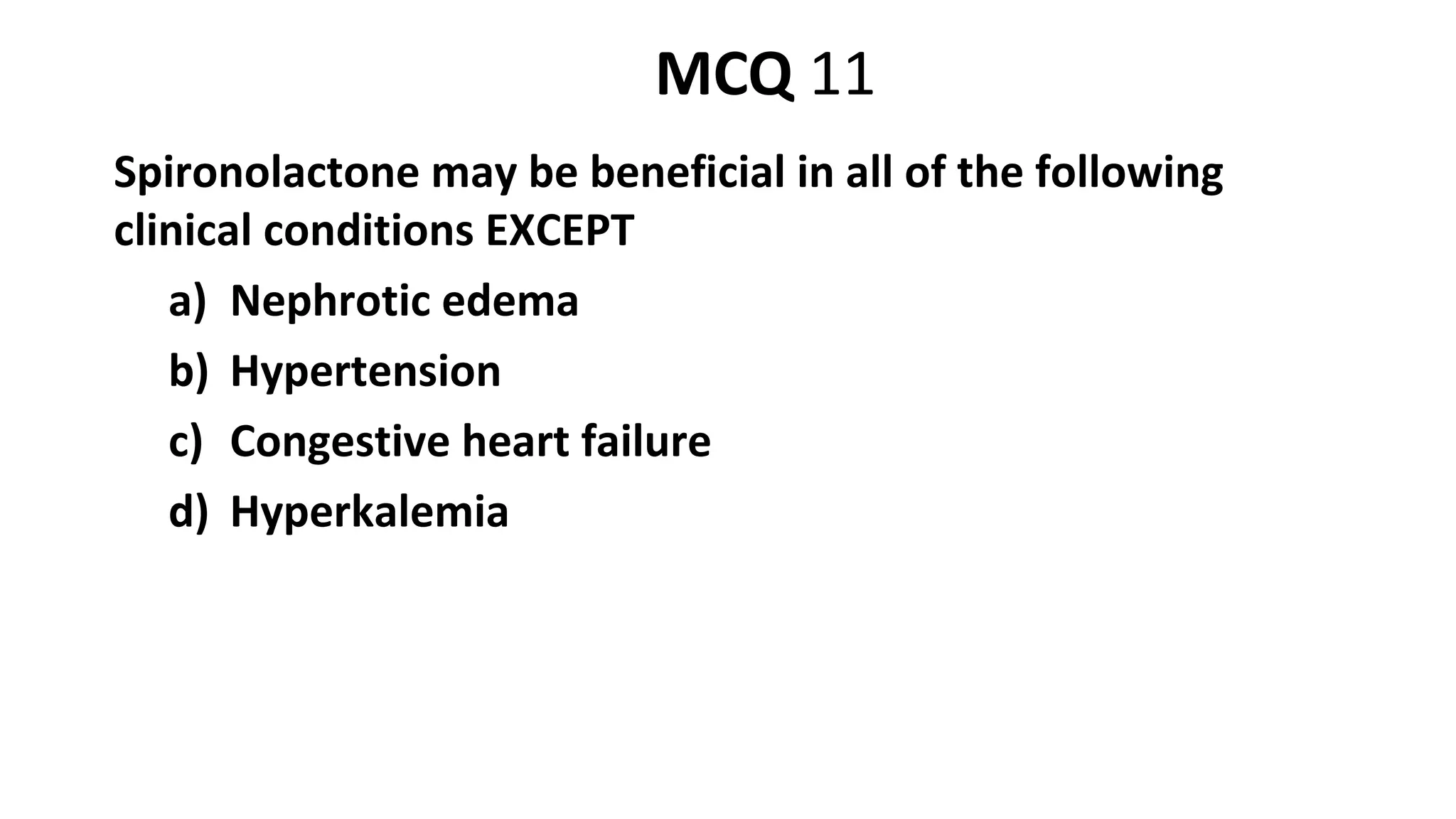
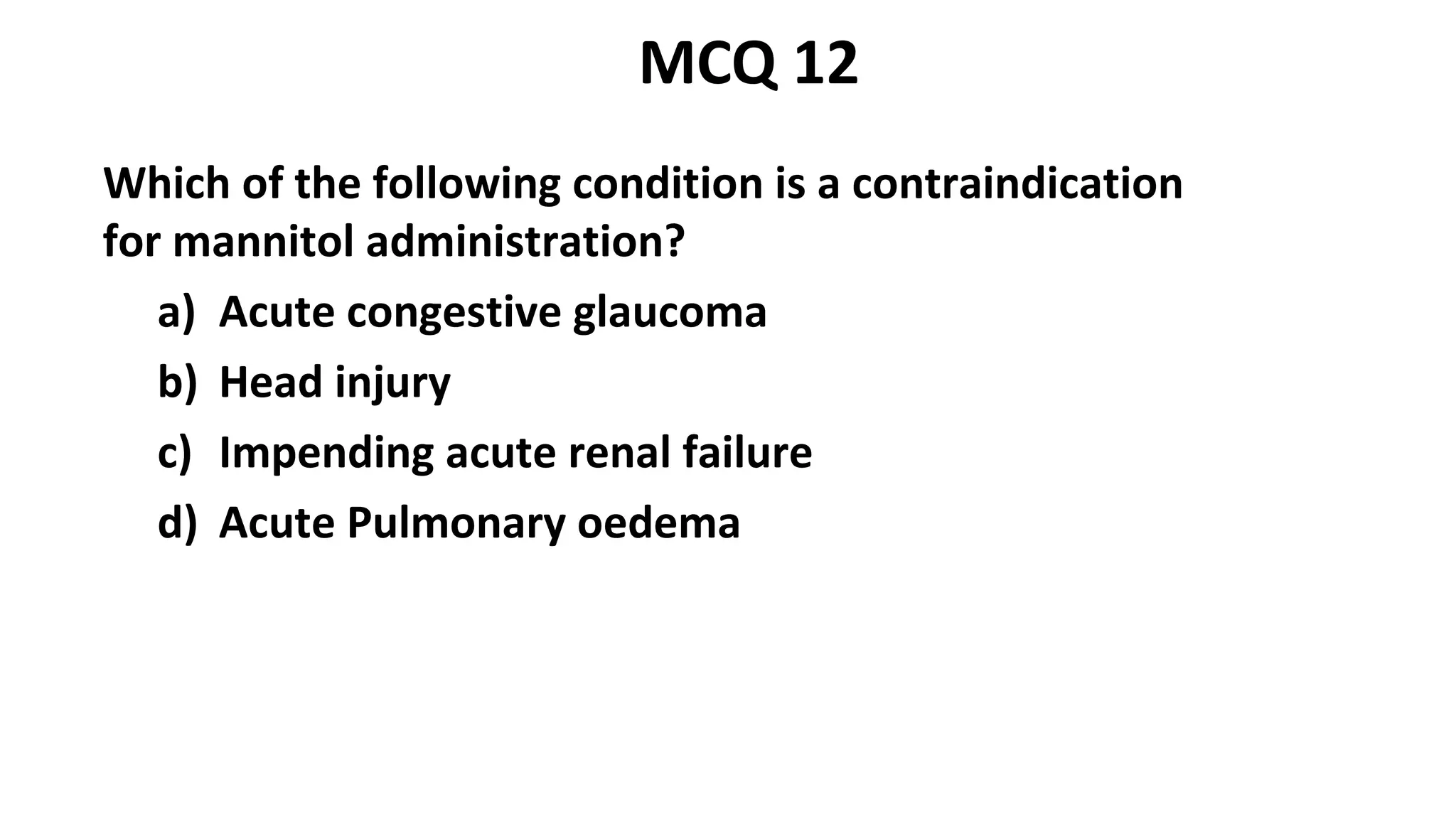
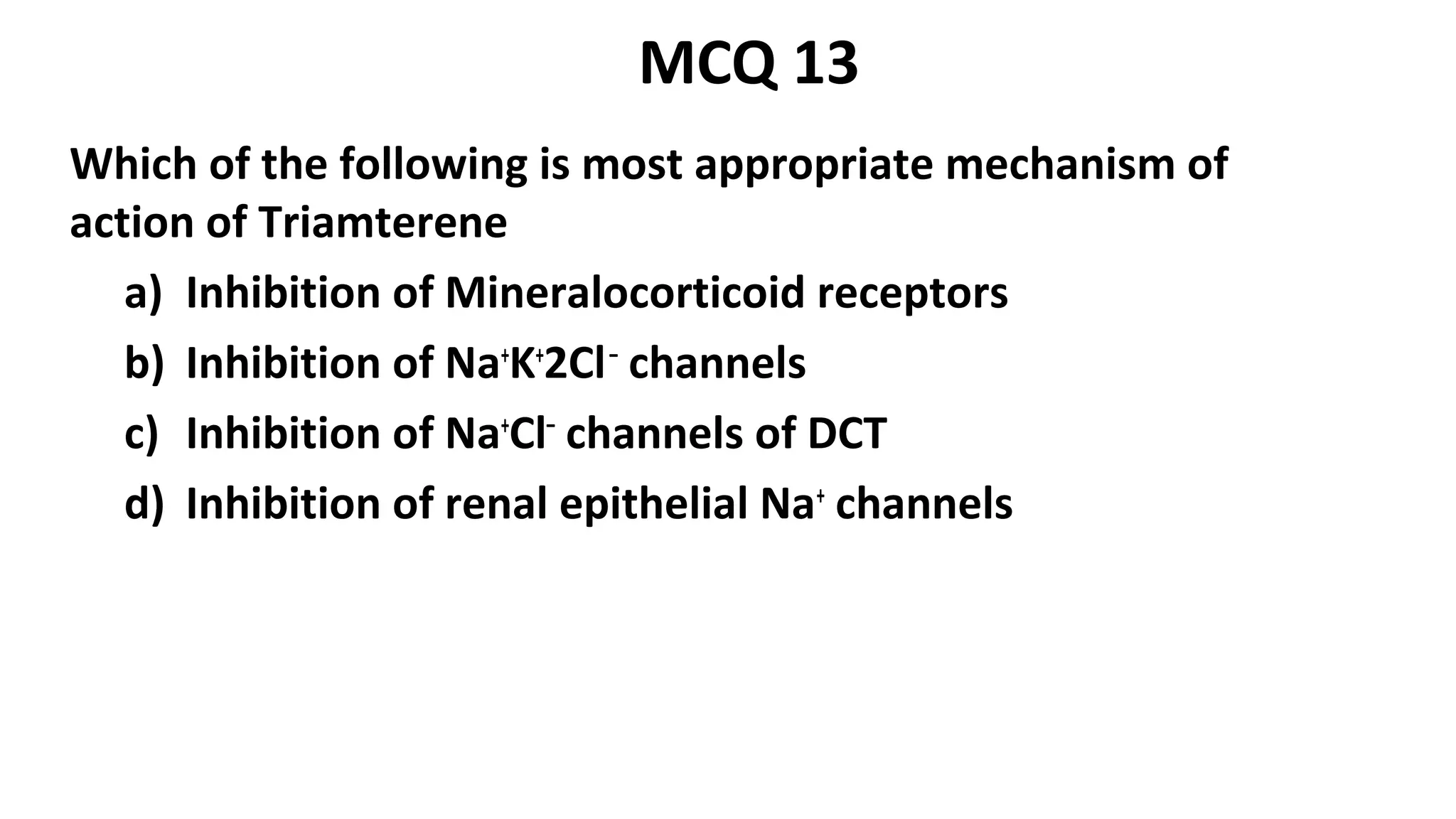
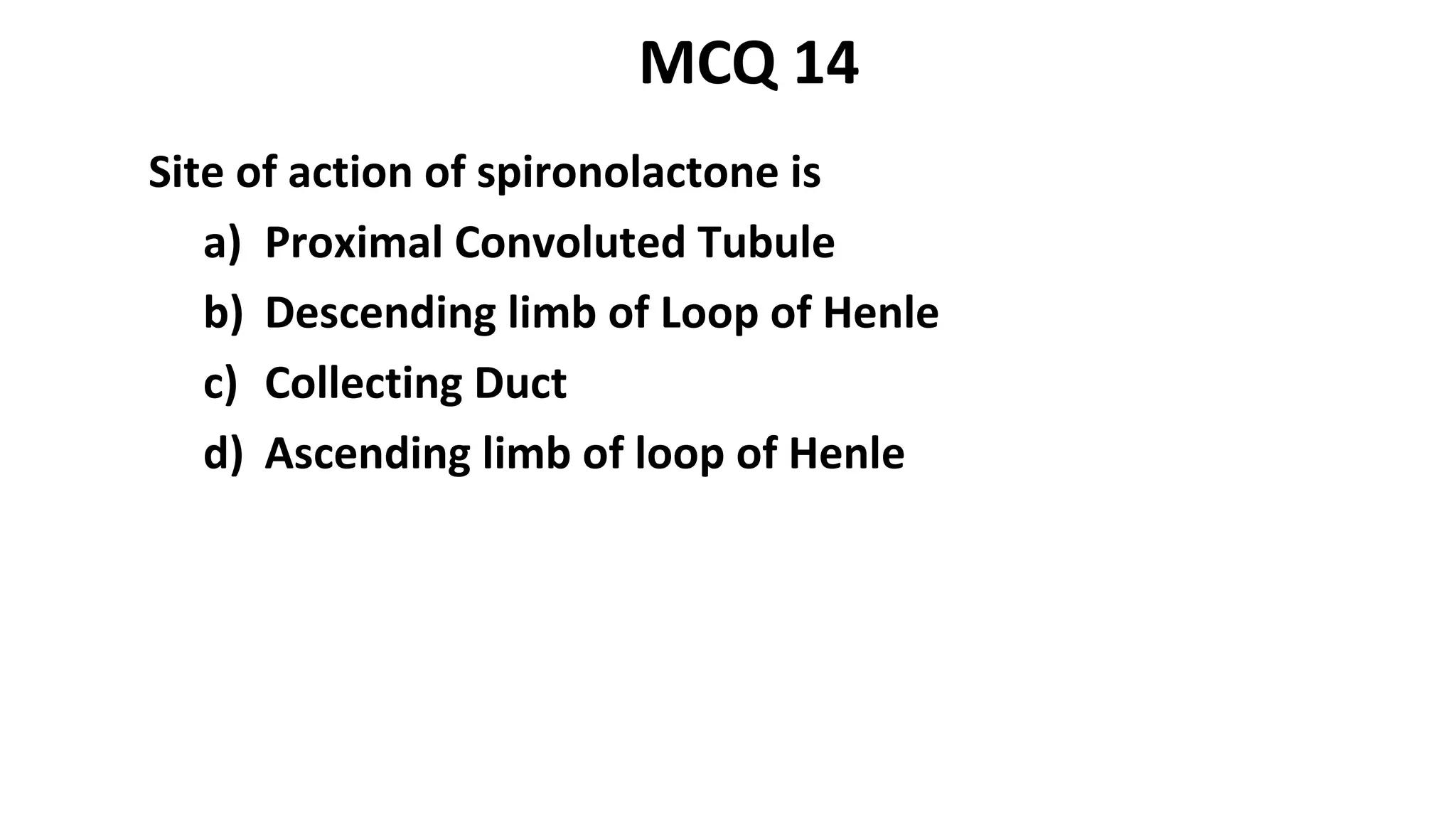
The document discusses various classes of diuretics including loop diuretics, thiazide diuretics, potassium sparing diuretics, carbonic anhydrase inhibitors, and osmotic diuretics. It focuses on the mechanisms of action, indications, and side effects of specific drugs within each class. It provides details on the pharmacology of spironolactone, amiloride, triamterene, acetazolamide, and mannitol. Clinical uses and precautions for different diuretics in conditions like edema, hypertension, heart failure, and kidney stones are also reviewed.