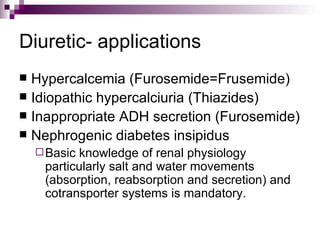
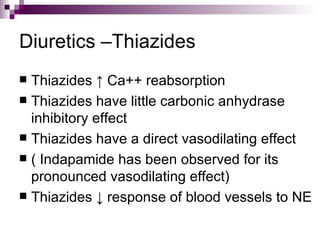
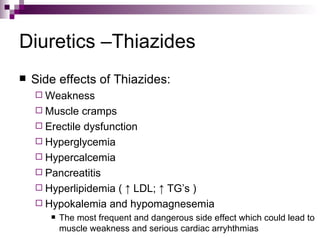
This document discusses diuretics, with a special focus on hydrochlorothiazide. It provides details on renal physiology and pharmacology. It describes the main types of diuretics and their mechanisms of action. It discusses thiazide diuretics in depth, including common examples like hydrochlorothiazide, their effects, kinetics, side effects, and clinical uses, especially for hypertension.