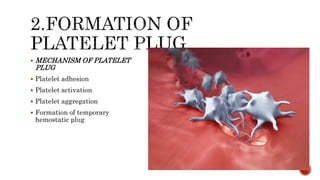
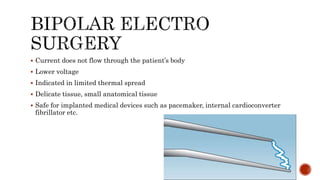
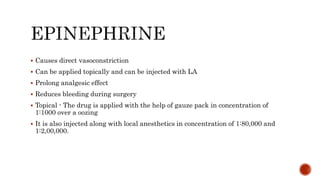
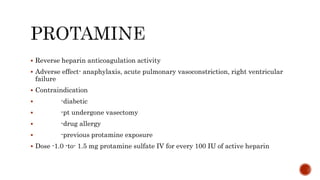
The document discusses hemostasis and mechanisms of bleeding control. It describes how hemostasis involves vascular constriction, platelet plug formation, and blood clotting in response to vascular injury. Multiple mechanisms are involved in clot formation, including platelet adhesion and aggregation, thrombin conversion of fibrinogen to fibrin, and fibrin mesh contraction. A variety of techniques can be used to achieve hemostasis, including direct pressure, gauze packing, sutures, staples, cautery, and pharmacological agents.