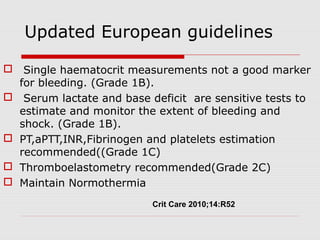
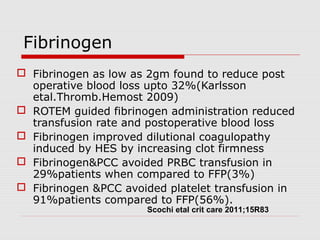
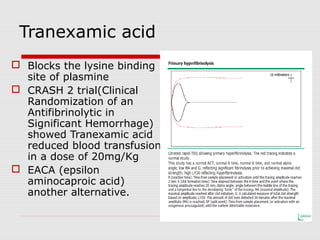
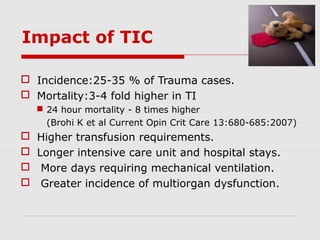
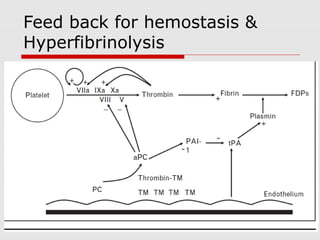
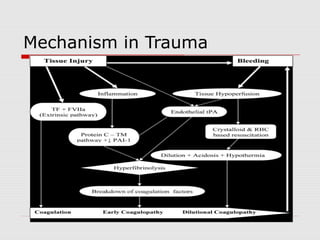
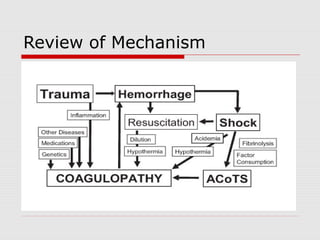
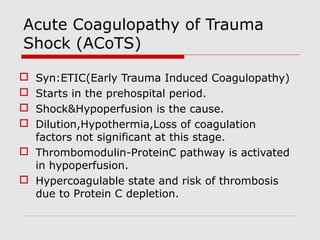
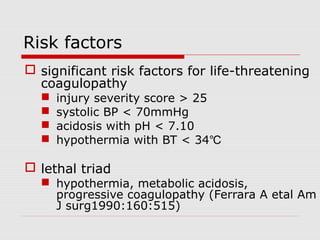
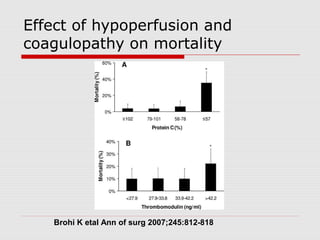
Trauma induced coagulopathy (TIC) starts early due to shock and hypoperfusion which activates the thrombomodulin-protein C pathway. TIC is associated with higher mortality, transfusion requirements, and organ dysfunction. Assessment of TIC requires thromboelastometry rather than standard coagulation tests due to confounding factors like hypothermia, acidosis, and dilution of clotting factors from fluid resuscitation. Treatment focuses on replacing depleted clotting factors, with fibrinogen and prothrombin concentrates highly recommended, as well as consideration of antifibrinolytics and recombinant factor VIIa in specific cases.


![Changes in fibrinogen synthesis and breakdown in pigs
after haemorrhage, hypothermia, and acidosis.
Fries D , Martini W Z Br. J. Anaesth. 2010;105:116-121
© The Author [2010]. Published by Oxford University Press on behalf of the British Journal of
Anaesthesia. All rights reserved. For Permissions, please email:
journals.permissions@oxfordjournal.org
Role of Fibrinogen](https://image.slidesharecdn.com/traumainducedcoagulopathy-130906005850-/85/Trauma-induced-coagulopathy-13-320.jpg)