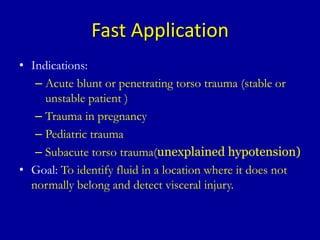
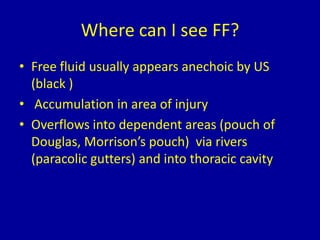
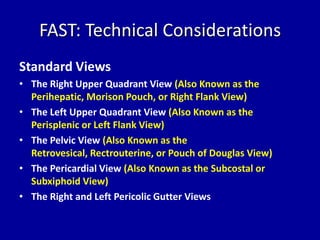
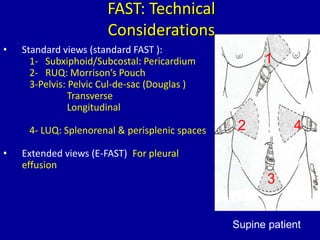
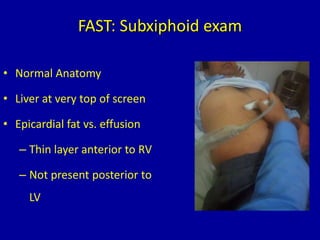
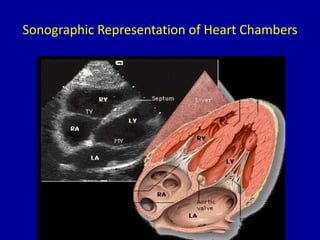
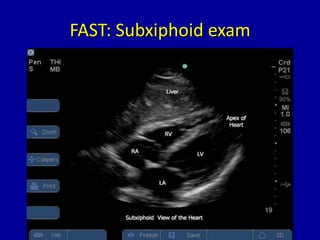
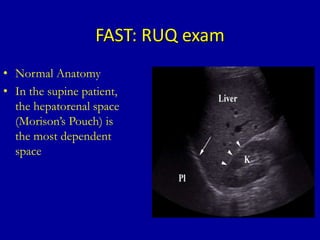
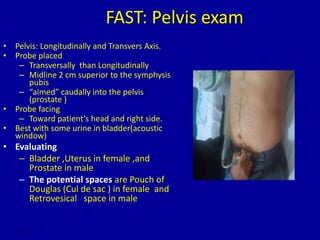
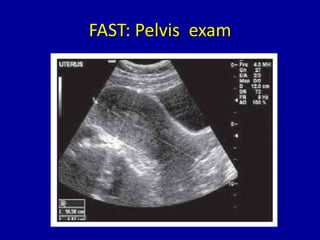
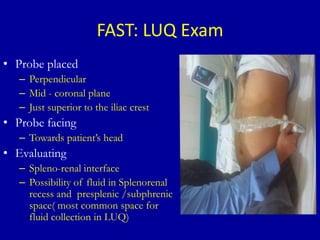
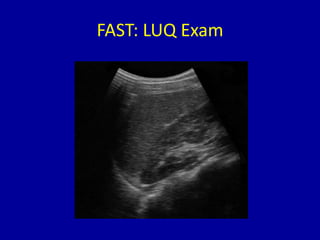
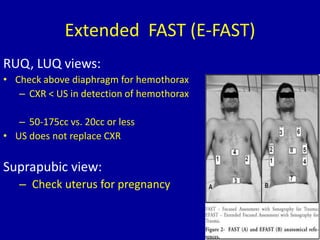
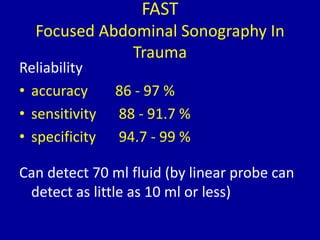
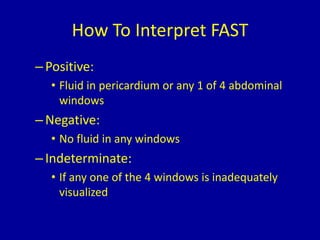
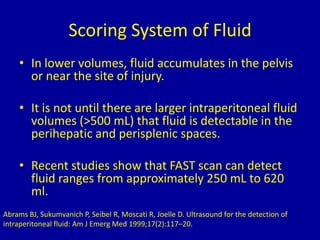
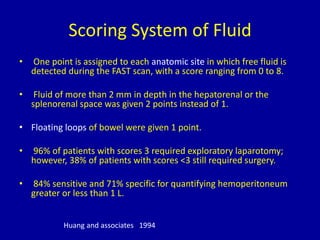
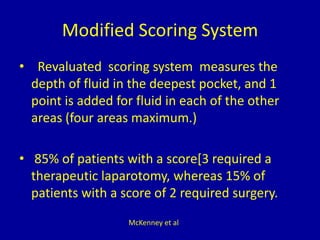
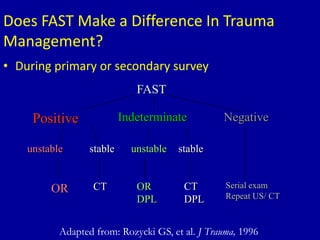
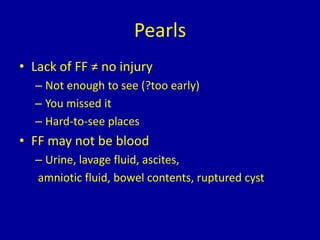
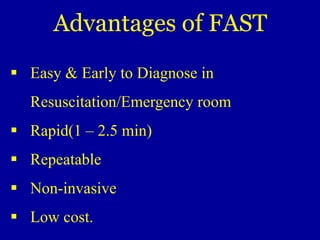
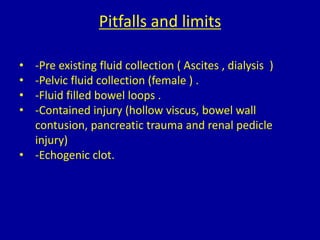
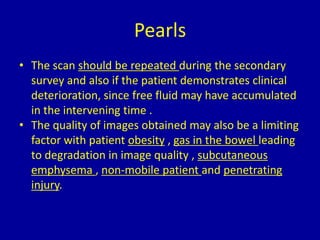
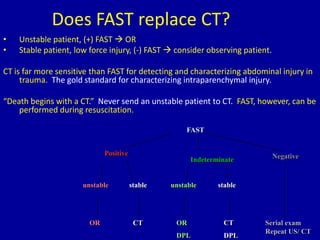
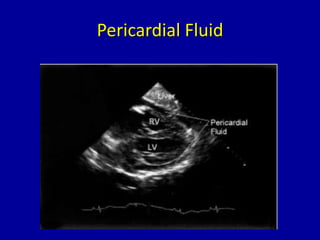
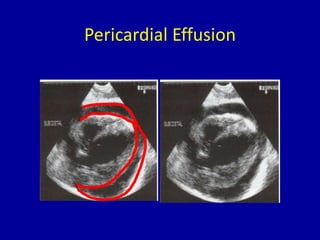
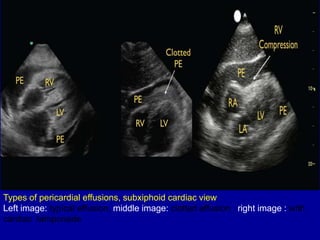
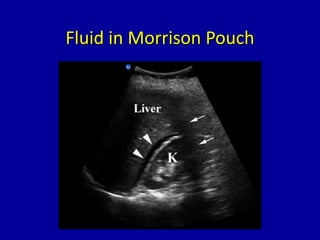
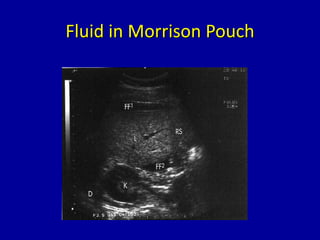
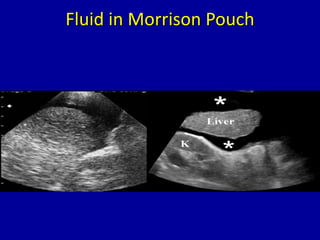
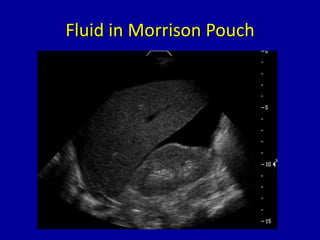
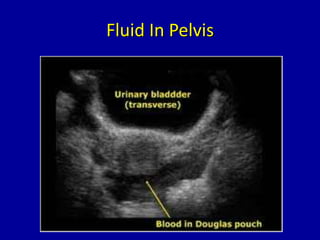
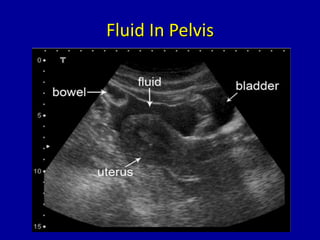
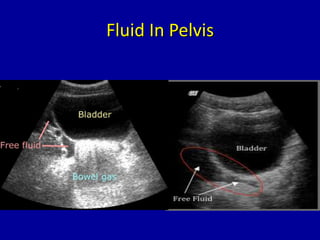
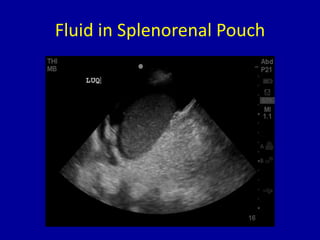
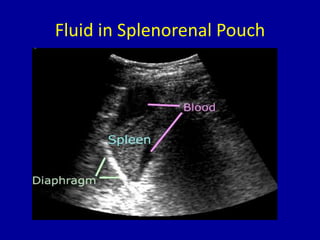
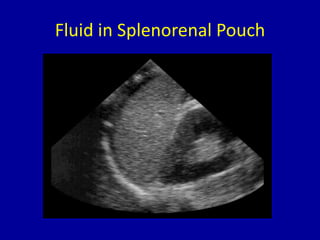
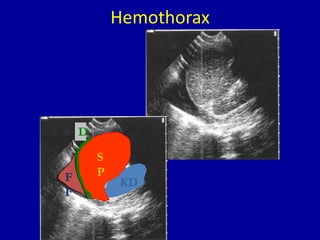
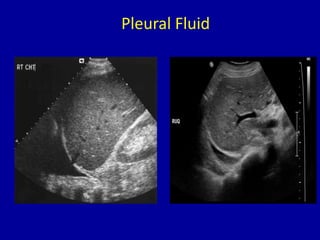
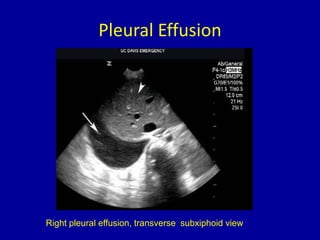
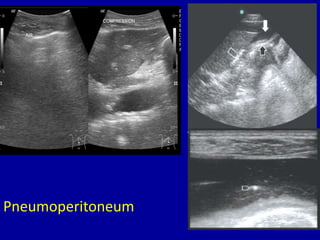
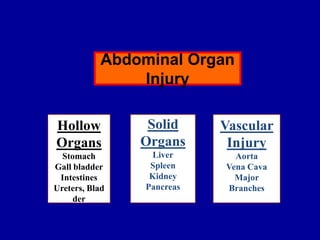
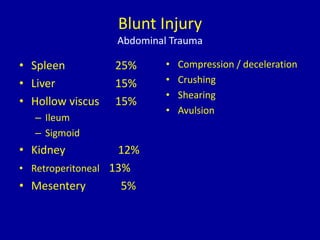
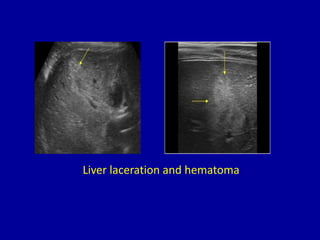
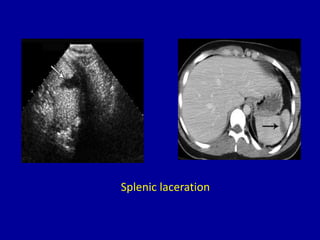
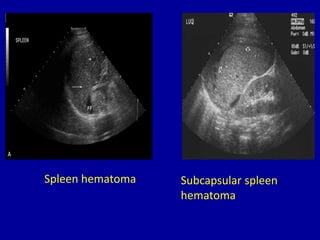
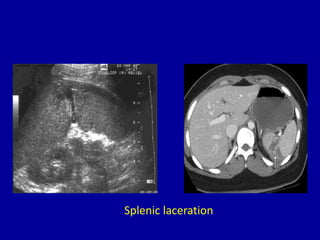
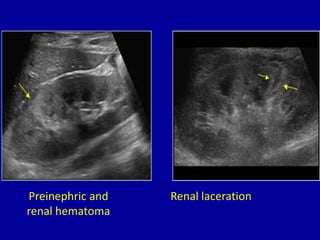
The document provides information about FAST (Focused Assessment with Sonography in Trauma) scans. It begins with an overview of what a FAST scan is used for - to identify fluid in the abdomen or pelvis where it is not normally found, which can indicate injury. It then details the anatomy visualized in a standard FAST scan and describes the technique. Examples are provided of free fluid appearing in different locations like Morrison's pouch or the pelvis. The document discusses interpreting FAST scans and explores limitations and advantages of the procedure. In under 3 sentences, the document provides an overview of the FAST scan for trauma patients to quickly identify free fluid that could indicate internal injury.