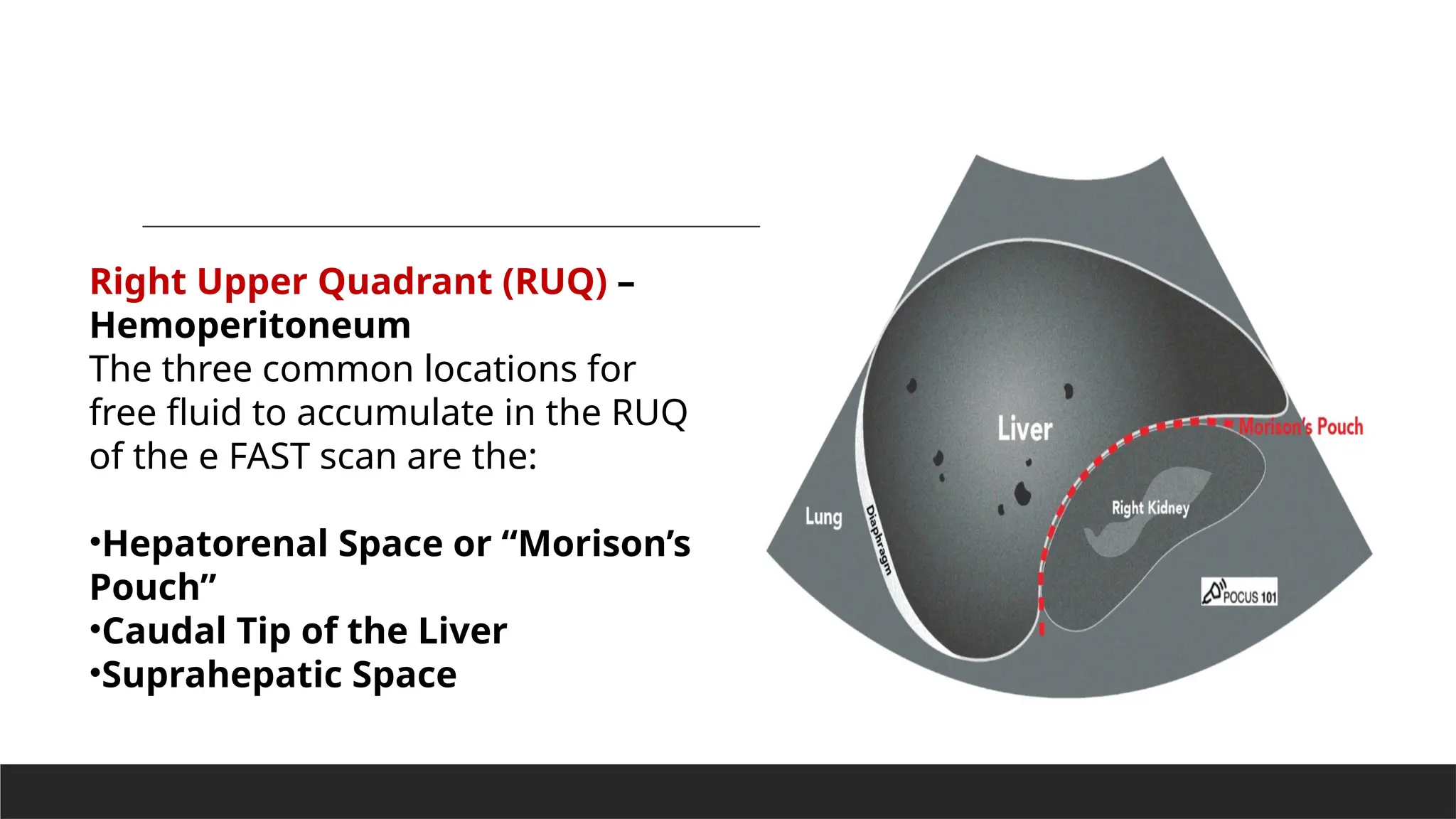
The document provides a detailed overview of the Focused Assessment with Sonography for Trauma (FAST) scan, outlining its purpose, indications, limitations, and patient preparation. It describes the procedural steps and views necessary to assess for free fluid in the abdomen, thorax, and cardiac regions, and how to utilize ultrasound techniques for effective diagnosis. It emphasizes the scan's critical role in trauma settings, particularly for identifying hemoperitoneum, hemothorax, and pneumothorax, along with their associated ultrasound findings.