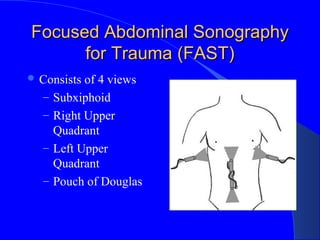
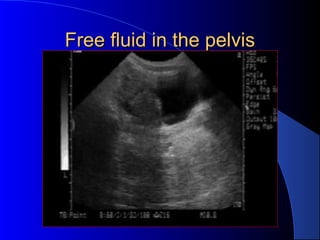
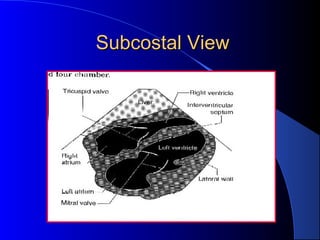
This document discusses the use of emergency ultrasound in trauma patients. It presents a clinical case of a 62-year-old male who slipped on ice and experienced pain in his lower chest. Bedside ultrasound revealed a liver laceration and 500cc of blood in the peritoneal cavity. The document then reviews diagnostic modalities for blunt abdominal trauma such as diagnostic peritoneal lavage, CT scan, and focused assessment with sonography for trauma (FAST). It provides details on performing and interpreting the FAST exam, including views of the right upper quadrant, left upper quadrant, and pelvis. The document concludes with a discussion of using ultrasound to detect occult penetrating cardiac trauma.