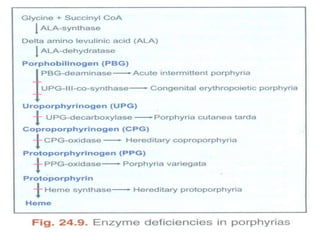
This document provides information on heme synthesis and disorders of heme synthesis (porphyrias). It describes the 7 step process of heme biosynthesis, which takes place partly in the cytoplasm and mitochondria. The key steps involve the formation of porphobilinogen (PBG), uroporphyrinogen, coproporphyrinogen, protoporphyrinogen, and finally heme through the insertion of iron. Regulation and some specific porphyrias are also outlined, including acute intermittent porphyria, congenital erythropoietic porphyria, porphyria cutanea tarda, hereditary coproporphyria, and variegate porphyria.