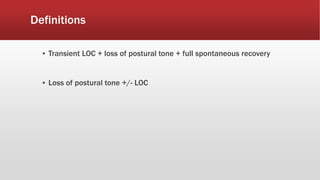
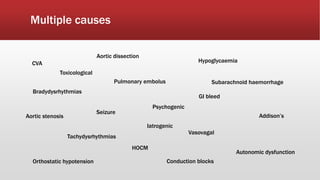
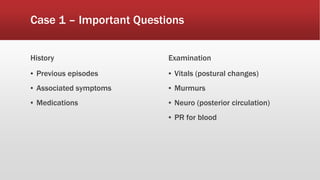
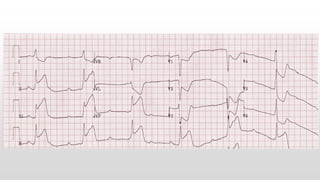
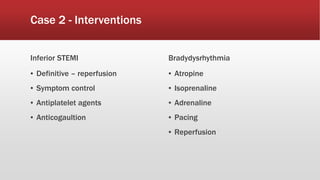
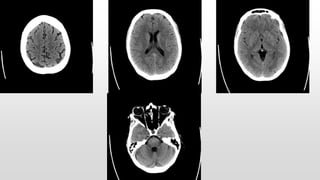
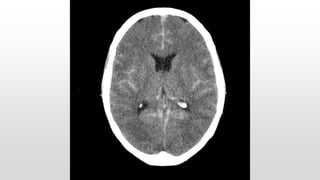
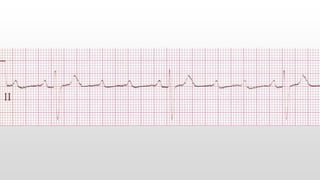
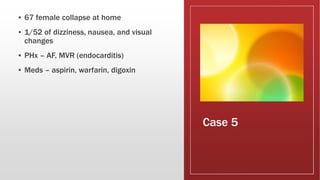
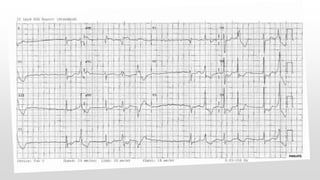
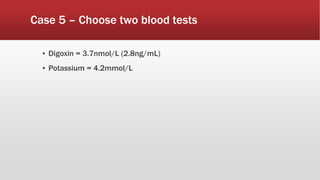
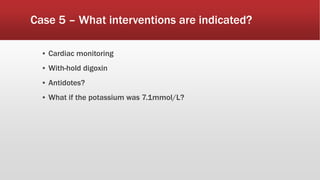
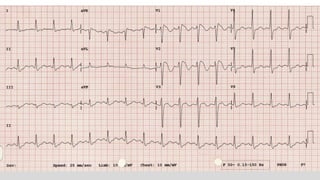
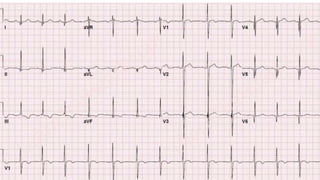
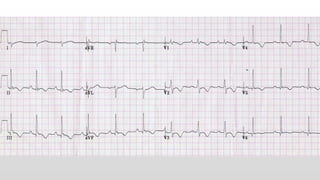
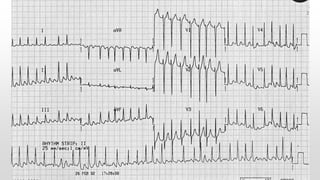
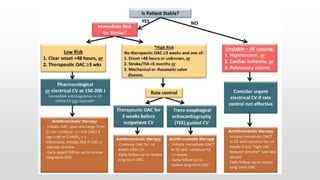
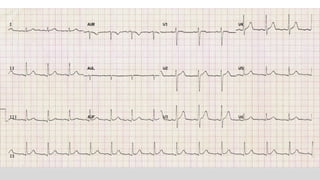
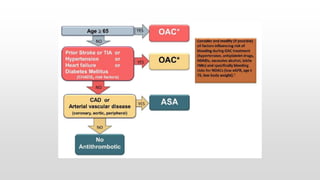
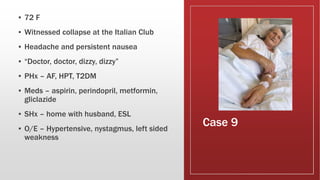
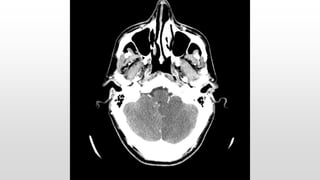
This document discusses various cases of collapse and syncope. It defines collapse as transient loss of consciousness with loss of postural tone and full recovery. Syncope is defined as loss of postural tone with or without loss of consciousness and full recovery. It then discusses the multiple potential causes of collapse and syncope including toxicological, cardiac conduction abnormalities, structural cardiac issues, autonomic dysfunction and more. It then goes through 9 case examples, discussing important questions to ask, potential tests and interventions for each case.