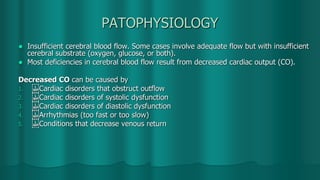
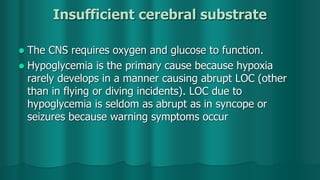
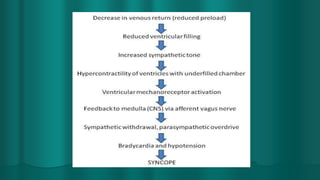
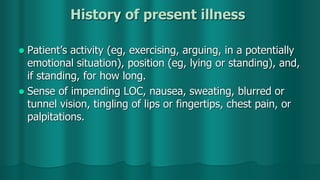
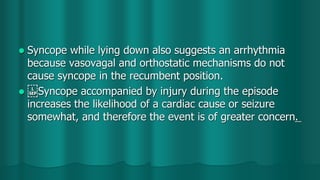
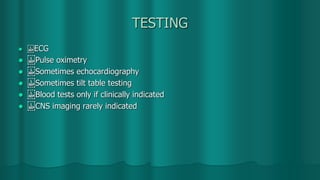
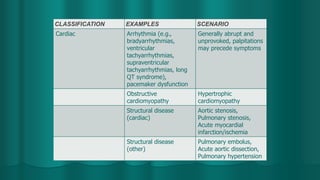
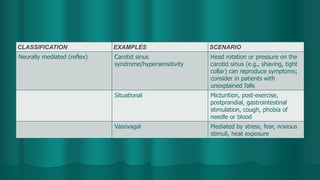
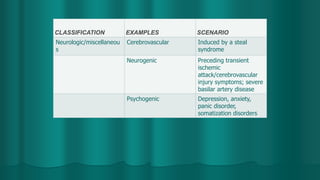
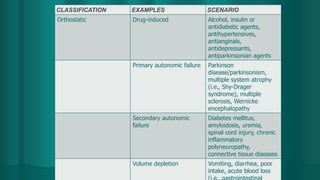
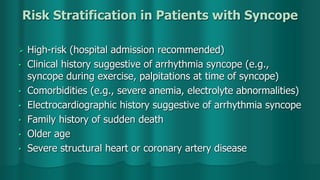
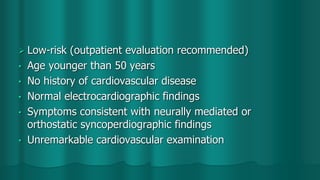
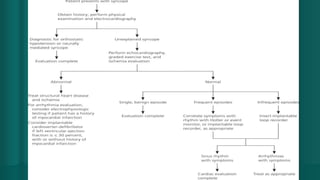
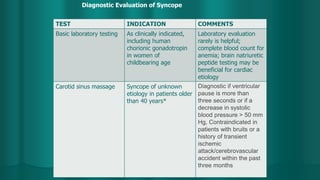
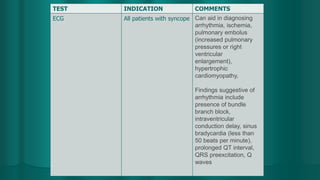
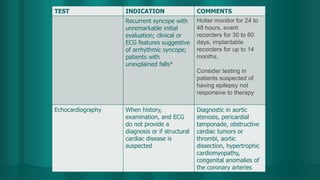
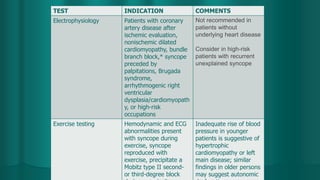
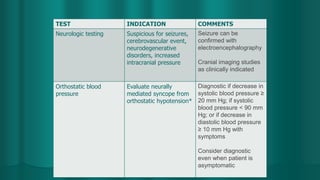
Syncope, or fainting, is caused by insufficient blood flow to the brain. It is usually brief and self-limited. Evaluation of syncope involves obtaining a detailed history, physical exam, ECG, and testing based on risk factors. Causes are categorized as benign if due to things like vasovagal response, or dangerous if due to cardiac arrhythmias. High-risk patients warrant further cardiac workup and monitoring, while low-risk patients can often be evaluated as outpatients.