This document discusses trauma management according to the EMST (Early Management of Severe Trauma) approach. Key points include:
1. EMST provides a systematic, stepwise approach to identify and treat life-threatening injuries before progressing to less severe issues.
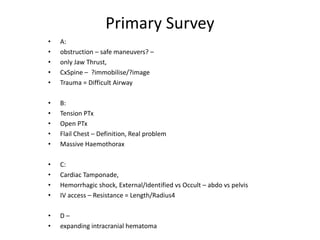
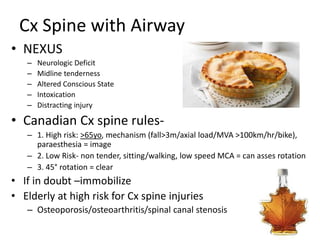
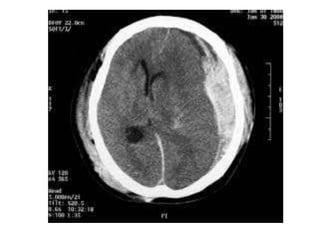
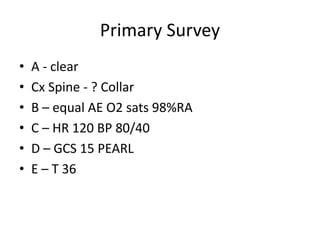
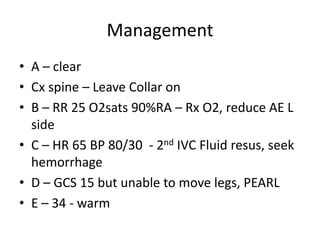
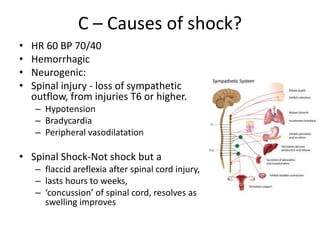
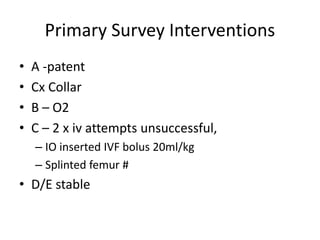
2. The primary survey focuses on airway, breathing, circulation, disability, and exposure to address critical life-saving interventions.
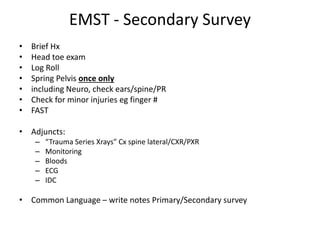
3. Secondary surveys involve a more thorough head-to-toe examination, imaging, and monitoring to identify less severe injuries.
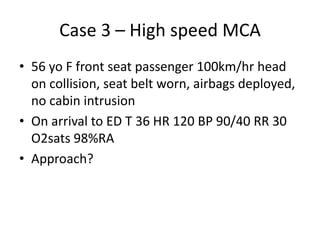
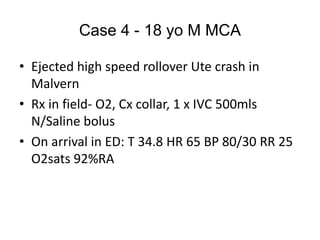
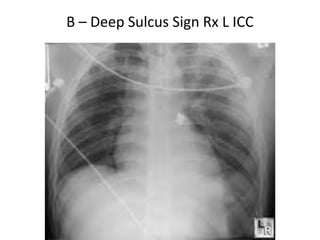
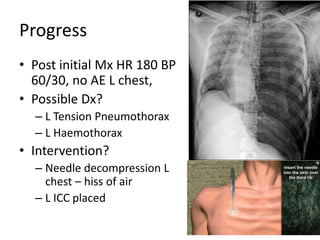
4. Several case examples are provided to demonstrate applying the EMST approach and managing specific trauma scenarios like hemorrhagic shock, spinal injuries, and tension pneumothor